


 النبات
النبات
 الحيوان
الحيوان
 الأحياء المجهرية
الأحياء المجهرية
 علم الأمراض
علم الأمراض
 التقانة الإحيائية
التقانة الإحيائية
 التقنية الحيوية المكروبية
التقنية الحيوية المكروبية
 التقنية الحياتية النانوية
التقنية الحياتية النانوية
 علم الأجنة
علم الأجنة
 الأحياء الجزيئي
الأحياء الجزيئي
 علم وظائف الأعضاء
علم وظائف الأعضاء
 الغدد
الغدد
 المضادات الحيوية
المضادات الحيويةRespiration
Respiration refers to the mechanisms for obtaining oxygen from the air and delivering it to the tissues, while eliminating carbon dioxide from the body. It is related to cellular respiration, the biochemical processes that consume this oxygen and generate the carbon dioxide in the course of making adenosine triphosphate (ATP). Respiration in the former sense involves four processes: (1) breathing, or ventilation of the lungs; (2) gas exchange between air and blood in the lungs; (3) gas transport in the blood; and (4) gas exchange between the blood and target tissues.
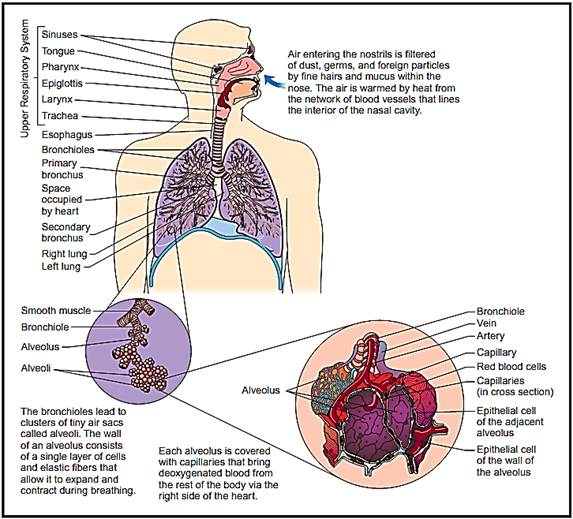
The human respiratory system.
Respiratory Anatomy
The respiratory system consists of: (1) the nasal cavity, which warms, cleans, and humidifies inhaled air; (2) the pharynx, where the respiratory and digestive systems meet and then diverge again; (3) the larynx, or voice box, which contains the vocal cords; (4) the trachea, or windpipe, a tube about 12 centimeters (4.7 inches) long and 2.5 centimeters (just less than an inch) wide that passes behind the heart and branches like a Y at its lower end; (5) bronchi and bronchioles, air tubes that begin at the fork of the trachea and divide into smaller and smaller divisions within each lung; and (6) alveoli, millions of tiny air sacs in the lung.
Except in the walls of the bronchi and bronchioles, the lungs have no muscle; they do not pump air in and out of themselves like the heart pumping blood, but are passively ventilated as the chest expands and contracts. The muscles that drive pulmonary ventilation are the diaphragm, a sheet of muscle between the thoracic and abdominal cavities; the intercostal muscles between the ribs; and other muscles of the abdomen and thorax that aid the primary respiratory muscles.
Pulmonary Ventilation
Ventilation is a rhythmic process, like the heartbeat, but its pacemakers are in the brainstem rather than in the chest. The medulla oblongata of the brainstem contains an inspiratory center composed of neurons that send signals to the diaphragm and external intercostal muscles. When these muscles are stimulated, they contract and enlarge the thoracic cavity. This creates a partial vacuum in the lungs. With the atmospheric pressure outside the body now greater than the pressure in the lungs, air flows “downstream” into the lungs and inflates them.
Usually no muscular effort is needed to exhale. When these muscles stop contracting, the elasticity of the thoracic cage (ribs, cartilages, diaphragm, and ligaments) causes it to spring back by itself, squeezing air out of the lungs. When one needs to exhale more deeply, however, the expiratory center of the medulla sends signals to the internal intercostal muscles, which pull the ribs downward and produce an extra degree of chest compression. The abdominal muscles also aid by increasing pressure in the abdominal cavity, pushing up on the diaphragm. These muscles are important in public speaking, singing, shouting, playing wind instruments, and blowing out candles, for example.
In normal, relaxed breathing, most adults inhale a tidal volume averaging 500 milliliters (16.9 fluid ounces) of air in each respiratory cycle. With maximum effort, however, one can inhale a greater amount called the vital capacity, averaging about 4,700 milliliters (almost 159 fluid ounces) in adults.
Pulmonary Gas Exchange
About 70 percent of the air a person inhales fills the millions of alveoli in the lungs. Each alveolus is surrounded by a basketlike mesh of blood capillaries. The wall separating the inhaled air from the blood is only 0.5 micrometer thick—only one-fifteenth the diameter of a single red blood cell—so it presents very little barrier to gas diffusion between the air and blood.
Oxygen has a concentration (partial pressure) of 104 mmHg in the alveolar air and 40 mmHg in the arriving capillary blood. Thus, it diffuses down its concentration gradient from the air, through the alveolar wall, into the blood. About 98.5 percent of this oxygen binds to the pigment hemoglobin in the red blood cells, and the other 1.5 percent dissolves in the blood plasma.
Carbon dioxide (CO2), has a partial pressure of 46 mmHg in the arriving blood and 40 mmHg in the alveolar air, so its concentration gradient dictates that it diffuses the other way, from blood to air, and is then exhaled. About 70 percent of this CO2 comes from the breakdown of carbonic acid in the blood; 23 percent from CO2 bound to hemoglobin, albumin, and other blood proteins; and 7 percent from gas dissolved in the blood plasma.
Gas Transport
Blood leaving the lungs is therefore relatively high in O2 (oxygen in its diatomic form) and low in CO2. It travels via the pulmonary veins to the left side of the heart, which pumps it out into the systemic circulation. This division of the circulatory system delivers it to every organ of the body.
Systemic Gas Exchange
When the blood reaches the systemic blood capillaries, gases undergo processes that are essentially the reverse of what occurs in the pulmonary alveoli. The blood unloads O2, which diffuses into the tissue fluid and thus reaches the cells around the blood capillaries. At the same time, the CO2 generated by the metabolism of those cells diffuses into the blood to be carried away to the lungs for disposal.
Blood typically contains 95 mmHg O2 upon arrival at the systemic capillaries and 40 mmHg O2 upon leaving. Conversely, the blood has 40 mmHg of CO2 on arrival at the systemic capillaries and typically 46 mmHg CO2 when it leaves. The blood does not, however, unload the same amount of O2 to all tissues or pick up the same amount of CO2. The more active a tissue is, the warmer it is, the lower its O2 level is, and the lower its pH is (because it generates more CO2 and CO2 reduces the pH of body fluids). Heat, low O2, low pH, and other factors enhance O2 unloading and CO2 loading, so tissues that need the most oxygen and waste removal get more than less active tissues do. The biochemistry of hemoglobin is mainly responsible for this elegant adjustment of gas exchange to the individual needs of different tissues.
References
Ganong, William F. Review of Medical Physiology, 19th ed. Stamford, CT: Appleton and Lange, 1999.
Saladin, Kenneth S. Anatomy and Physiology—The Unity of Form and Function, 2nd ed. Dubuque, IA: McGraw-Hill, 2001.



|
|
|
|
دخلت غرفة فنسيت ماذا تريد من داخلها.. خبير يفسر الحالة
|
|
|
|
|
|
|
ثورة طبية.. ابتكار أصغر جهاز لتنظيم ضربات القلب في العالم
|
|
|
|
|
|
|
قسم شؤون المعارف ووفد من جامعة البصرة يبحثان سبل تعزيز التعاون المشترك
|
|
|