
Breast
 المؤلف:
Kelly M. Harrell and Ronald Dudek
المؤلف:
Kelly M. Harrell and Ronald Dudek
 المصدر:
Lippincott Illustrated Reviews: Anatomy
المصدر:
Lippincott Illustrated Reviews: Anatomy
 الجزء والصفحة:
الجزء والصفحة:
 12-7-2021
12-7-2021
 10568
10568
Breast
The most prominent surface feature of the anterior thorax is the breast. Both males and females have breasts, although breast development and function differ between the sexes.
A. Embryology
During week 4, a pair of epidermal (ectoderm) thickenings called the mammary ridges form on both sides of the embryo. The mammary ridges extend from the axilla to the inguinal region. The mammary ridges normally disappear below the axilla in humans. During week 7, the mammary ridge at the site of the future breast forms a primary bud, which invaginates into the underlying dermis (mesoderm).
During week 10, the primary bud branches into several secondary buds. The secondary buds will lengthen and branch throughout the remainder of gestation and eventually canalize to form 15-25 lactiferous ducts. At birth, the mammary gland consists of 15-25 rudimentary lactiferous ducts that open into a small surface depression called the mammary pit. The mammary pit is converted to an averted nipple as the underlying dermis (mesoderm) proliferates within a few weeks after birth. The skin surrounding the nipple forms the areola (Fig. 1).
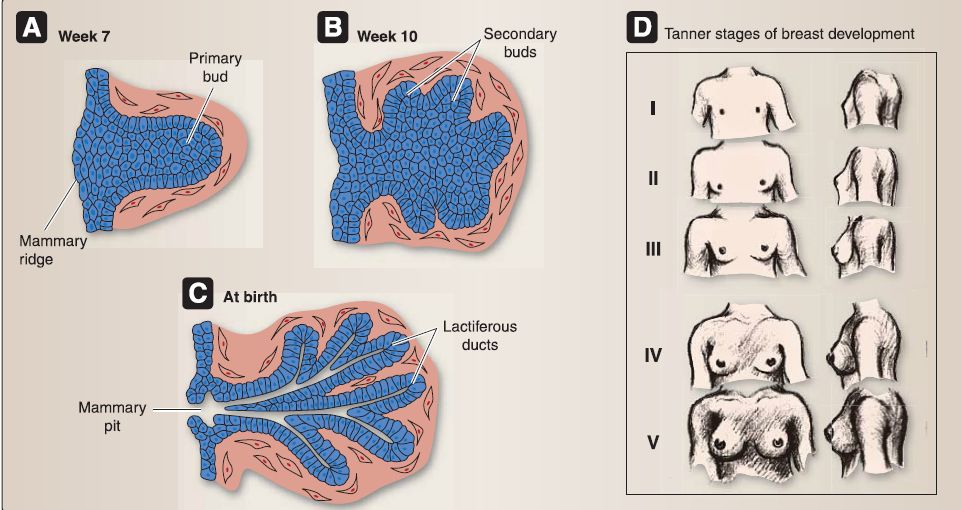
Figure 3.9: Embryology of breast. A, Week 7. B, Week 10. C, At birth. D, Tanner stages of breast development.
B. Anatomy
Although present in both males and females, breasts are more prominent in females as they contain well-developed mammary glands and variable amounts of adipose tissue.
1. Mammary glands: These are arranged into lobules (15-25) within the female breast. Lobules are supported by suspensory ligaments (Cooper's ligaments) that anchor into the overlying dermis.
Mammary glands in men are nonfunctional. The female breast is in the superficial fascia of the chest, typically between the 2nd and 6th intercostal spaces, overlying the deep pectoral fascia and pectoralis major and minor muscles (Fig. 2).
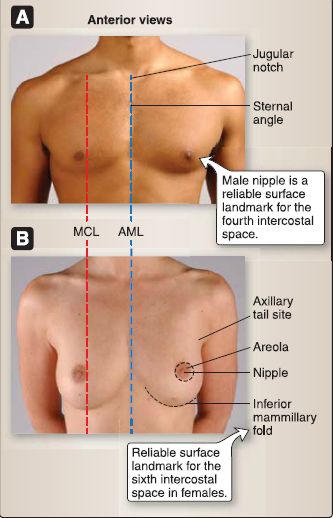
Figure 2 : Breast. A, Male. B, Female. AML = anterior median line, MCL = midclavicular line.
2. External features: These include the nipple and areola. The nipple is surrounded by the pigmented circular areola and can vary in size and prominence. The male nipple serves as a reliable landmark for the 4th intercostal space. However, due to the varying amounts of adipose in the female breast, the nipple is not a reliable surface landmark. Rather, the inferior mammillary fold (inferior cutaneous crease) is often used to locate the 6th intercostal space in the female.
C. Histology
The mammary gland within the breast is a compound, tubuloalveolar gland that develops as downgrowths of the skin epidermis along the milk line, which runs from the axilla to the groin on each side of the torso. The mammary gland remains inactive until pregnancy, during which time the mammary gland matures functionally and morphologically. This maturation is controlled by estrogen, progesterone, prolactin, and placental lactogen (Fig. 3 ).
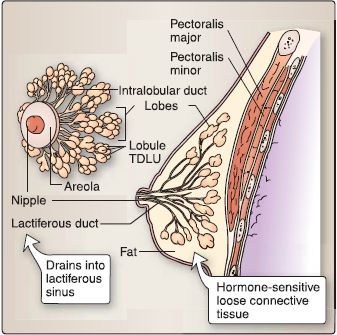
Figure 3 : Organization of mammary gland. TDLU = Terminal ductule lobular unit.
1. Composition: The mammary gland is composed of 15-25 irregularshaped lobes that are separated from each other by dense, irregular connective tissue and adipose tissue. Within each lobe, there are numerous lobules or terminal ductule lobular units (TDLUs). A TDLU comprises a cluster of terminal ductules, hormonesensitive loose connective tissue, and an intralobular duct.
2. Ductal system: The alveoli surrounded by myoepithelial cells secrete milk, which empties into intralobular ducts lined by simple cuboidal epithelium and then into larger interlobular ducts lined by simple columnar epithelium. The interlobular ducts merge into 15-25 lactiferous sinuses lined by stratified cuboidal epithelium and then into 15-25 lactiferous ducts lined by keratinized stratified squamous epithelium. The lactiferous ducts open onto the tip of the nipple arranged in a ring.
3. Stages: At birth, the mammary gland consists of 15-25 rudimentary lactiferous ducts that open into a small surface depression called the mammary pit. The mammary gland remains relatively inactive until puberty, when the female progresses through basically four stages (Fig. 4).
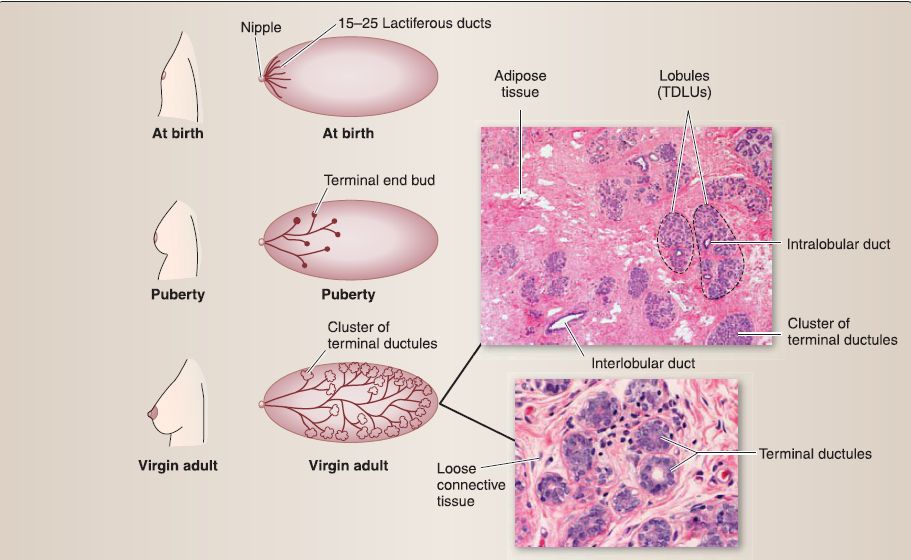 Figure 4: Histology of breast and mammary gland stages, birth through virgin adult. TDLUs = terminal ductule lobular units.
Figure 4: Histology of breast and mammary gland stages, birth through virgin adult. TDLUs = terminal ductule lobular units.
a. Puberty stage: During puberty, the duct system comprises a modest network of ducts that branch into the connective tissue and end with a terminal end bud. The terminal end bud is a mass of epithelial cells (i.e., no lumen).
b. Virgin adult stage: The duct system now comprises a fairly advanced network of branching ducts that have grown in length and end in a cluster of terminal ductules.
c. Pregnancy stage: During pregnancy, a prolific network of branching ducts have grown and elongated. This proliferation of the duct system takes place at the expense of the connective tissue and adipose tissue in the breast, which concurrently decreases during pregnancy (Figure 5). Eventually, the characteristic structure of the mammary gland takes shape, comprising numerous lobules or TDLUs, interlobular ducts, lactiferous sinuses, and lactiferous ducts.
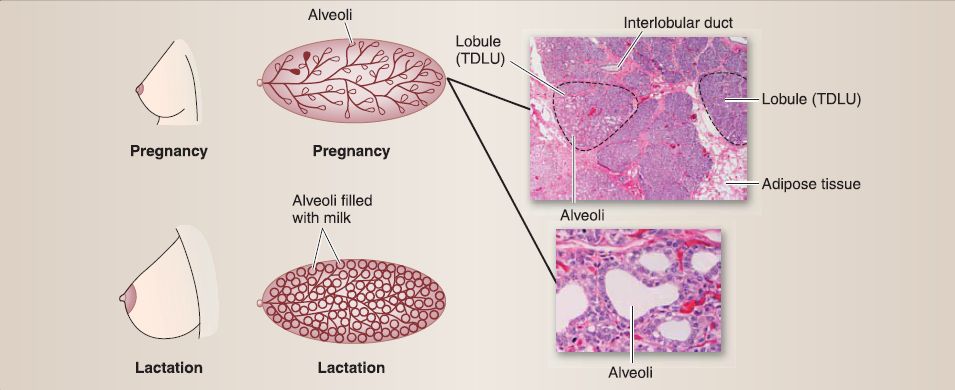 Figure 5 :Histology of breast and mammary gland stages, pregnancy, and lactation. TDLUs = terminal ductule lobular units.
Figure 5 :Histology of breast and mammary gland stages, pregnancy, and lactation. TDLUs = terminal ductule lobular units.
[1] Alveoli: In addition, the terminal ductules differentiate and form secretory alveoli that are surrounded by myoepithelial cells.
[2] Colostrum: The ducts and alveoli distend as alveoli secrete colostrum. Plasma cells, lymphocytes, and eosinophils infiltrate the connective tissue at this time.
d. Lactation stage: Because the alveoli become active in milk production and milk secretion at this stage, their lumina become filled with milk. Numerous lipid droplets and secretory granules containing dense aggregates of milk proteins can be observed ultrastructurally at the apical end of the alveolar epithelial cells. Human breast milk is produced 1-3 days after childbirth.
[1] Breast milk contents: Breast milk contains a substantial amount of lipid, protein, lactose, vitamins, and secretory immunoglobulin A (which affords temporary enteric passive immunity).
[2] Milk letdown: Although milk is produced continuously by the alveoli (milk production), it is delivered only in response to suckling (milk letdown). Suckling stimulates afferent neurons that relay the information to the hypothalamus such that the following actions occur: 1) oxytocin is released from the neurohypophysis, which causes the contraction of myoepithelial cells and milk letdown, and 2) prolactininhibiting hormone (dopamine} is inhibited, which causes the release of prolactin from the adenohypophysis and further milk production.
D. Vasculature
The breast receives arterial blood supply primarily from branches of the internal thoracic (medial mammary branches), lateral thoracic (lateral mammary branches), thoracoacromial (pectoral branches), and anterior intercostal (perforating branches) arteries. Venous drainage of the breast occurs mainly through tributaries of the axillary artery, with minimal drainage into the internal thoracic veins.
E. Lymphatics
Lymphatic drainage of the breast is very important to understand in the context of breast cancer metastasis. A network of lymphatic vessels drains the glandular tissue first into a delicate subareolar plexus, just deep to the nipple. The subareolar plexus is continuous with the circumareolar plexus, which communicates with the contralateral breast. Approximately 75% of lymph drainage travels laterally toward the axillary lymph nodes, particularly the pectoral group of nodes.
Lymph then travels proximally toward the subclavicular nodes and eventually into the right or left lymphatic duct. Approximately 25% of lymph drainage occurs medially by way of the parasternal nodes along the lateral borders of the sternum. These nodes also communicate to contralateral nodes, which may allow for metastasis from one breast to the other (Fig. 6).
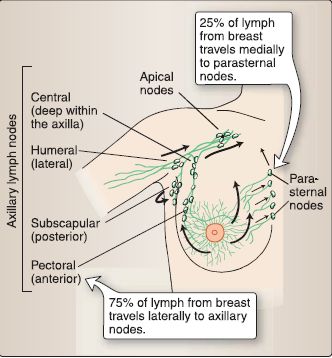
Figure 6: Breast lymphatic drainage. Black arrows indicate direction of flow.
F. Surface anatomy
Palpation of important surface landmarks in the thorax is often warranted during a thorough physical assessment. In addition, imaginary directional lines allow for consistent and reliable anatomical description in the thorax (Fig. 7).
1. Bony landmarks: Important bony landmarks include the following.
a. Sternoclavicular joint: This is used to assess musculoskeletal impairment.
b. Jugular (suprasternal) notch: This is used to assess aortic pathology.
c. Sternal angle: This is a demarcation between superior and inferior mediastinal regions.
2. Directional lines: These include the anterior midsternal lines; clavicular lines (bilateral); anterior, mid-, and posterior axillary lines; and the posterior median line (see Fig. 7).
3. Quadrants: For examination and diagnostic purposes, the breast is divided into four quadrants: superior lateral (with axillary process), superior medial, inferior lateral, and inferior medial. Imaginary vertical (12 o'clock-6 o'clock) and horizontal (9 o'clock-3 o'clock) lines are drawn through the middle of the nipple (Fig. 8).
d. Xyphoid process: The T6 dermatome overlies this process.
e. Costal margin: This is used to assess for hepatomegaly(iver enlargement).
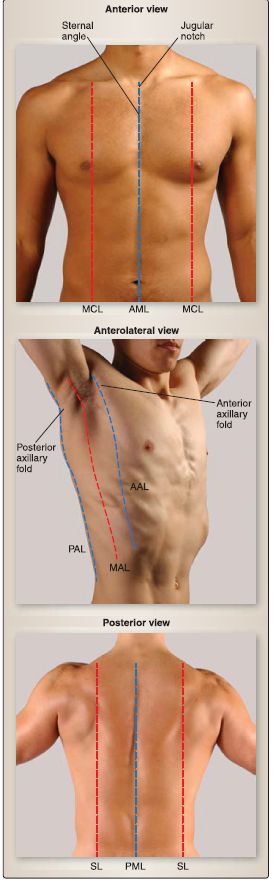
Figure 7: Thoracic surface anatomy. AAL = anterior axillary line, AML = anterior median line, MAL = midaxillary line, MCL = midclavicular line, PAL = posterior axillary line, PML = posterior median line, SL = scapular line.
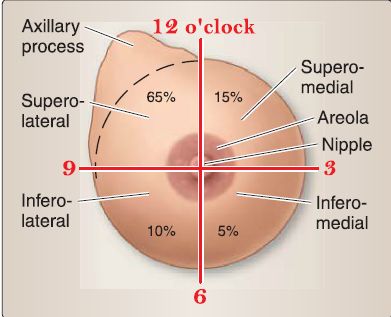
Figure 8: Breast quadrants. Percentages indicate incidence of pathology in each
quadrant.
 الاكثر قراءة في علم التشريح
الاكثر قراءة في علم التشريح
 اخر الاخبار
اخر الاخبار
اخبار العتبة العباسية المقدسة


