النبات

مواضيع عامة في علم النبات

الجذور - السيقان - الأوراق

النباتات الوعائية واللاوعائية

البذور (مغطاة البذور - عاريات البذور)

الطحالب

النباتات الطبية


الحيوان

مواضيع عامة في علم الحيوان

علم التشريح

التنوع الإحيائي

البايلوجيا الخلوية


الأحياء المجهرية

البكتيريا

الفطريات

الطفيليات

الفايروسات


علم الأمراض

الاورام

الامراض الوراثية

الامراض المناعية

الامراض المدارية

اضطرابات الدورة الدموية

مواضيع عامة في علم الامراض

الحشرات


التقانة الإحيائية

مواضيع عامة في التقانة الإحيائية


التقنية الحيوية المكروبية

التقنية الحيوية والميكروبات

الفعاليات الحيوية

وراثة الاحياء المجهرية

تصنيف الاحياء المجهرية

الاحياء المجهرية في الطبيعة

أيض الاجهاد

التقنية الحيوية والبيئة

التقنية الحيوية والطب

التقنية الحيوية والزراعة

التقنية الحيوية والصناعة

التقنية الحيوية والطاقة

البحار والطحالب الصغيرة

عزل البروتين

هندسة الجينات


التقنية الحياتية النانوية

مفاهيم التقنية الحيوية النانوية

التراكيب النانوية والمجاهر المستخدمة في رؤيتها

تصنيع وتخليق المواد النانوية

تطبيقات التقنية النانوية والحيوية النانوية

الرقائق والمتحسسات الحيوية

المصفوفات المجهرية وحاسوب الدنا

اللقاحات

البيئة والتلوث


علم الأجنة

اعضاء التكاثر وتشكل الاعراس

الاخصاب

التشطر

العصيبة وتشكل الجسيدات

تشكل اللواحق الجنينية

تكون المعيدة وظهور الطبقات الجنينية

مقدمة لعلم الاجنة


الأحياء الجزيئي

مواضيع عامة في الاحياء الجزيئي


علم وظائف الأعضاء


الغدد

مواضيع عامة في الغدد

الغدد الصم و هرموناتها

الجسم تحت السريري

الغدة النخامية

الغدة الكظرية

الغدة التناسلية

الغدة الدرقية والجار الدرقية

الغدة البنكرياسية

الغدة الصنوبرية

مواضيع عامة في علم وظائف الاعضاء

الخلية الحيوانية

الجهاز العصبي

أعضاء الحس

الجهاز العضلي

السوائل الجسمية

الجهاز الدوري والليمف

الجهاز التنفسي

الجهاز الهضمي

الجهاز البولي


المضادات الميكروبية

مواضيع عامة في المضادات الميكروبية

مضادات البكتيريا

مضادات الفطريات

مضادات الطفيليات

مضادات الفايروسات

علم الخلية

الوراثة

الأحياء العامة

المناعة

التحليلات المرضية

الكيمياء الحيوية

مواضيع متنوعة أخرى

الانزيمات
Fascia, Vasculature, Lymphatics, Innervation of upper limb
المؤلف:
Kelly M. Harrell and Ronald Dudek
المصدر:
Lippincott Illustrated Reviews: Anatomy
الجزء والصفحة:
21-7-2021
7386
Fascia, Vasculature, Lymphatics, Innervation of upper limb
Many structures in the upper limb can be described as either superficial or deep, including fascial layers, venous vessels, and lymphatic vessels and nodes. The following section describes the organization of these structures in addition to the arterial and nervous supply of the upper limb.
A. Superficial fascia
Deep to the skin of the upper limb lies a superficial fascia that contains varying amounts of loose connective and adipose tissues. Superficial veins, lymphatic vessels, and cutaneous nerves travel in this fascia, which is continuous with the superficial fascia of the neck and trunk.
B. Deep fascia
Deep to the superficial fascia is a deep fascia that is divided into several regions, including deltoid, pectoral, axillary, clavipectoral, brachia!, antebrachial, and palmar (Fig. 1). These deep fasciae are continuous with each other at different locations and collectively invest the upper limb muscle compartments. Medial and lateral intermuscular septa project internally to attach to bone and create the rigid compartments of the arm (anterior and posterior) and forearm (anterior and posterior).

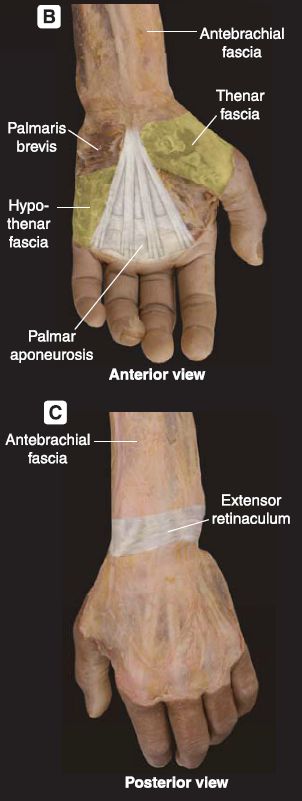
Figure 1: Fascia of the upper limb. A, Abducted upper limb showing continuity of fascia. B, Palmar aponeurosis. C, Dorsum of hand with extensor retinaculum.
1. Shoulder and arm fascia: The pectoral fascia covers the pectoralis major muscle and is continuous with the axillary fascia (Fig. 2). The clavipectoral fascia lies deep to the pectoralis major muscle, encapsulates the pectoralis minor and subclavius muscles, and is continuous superiorly with the deep cervical fascia. Continuous with the deltoid, pectoral, and axillary fascia is the brachial fascia, which contains the muscles of the arm in anterior and posterior compartments.
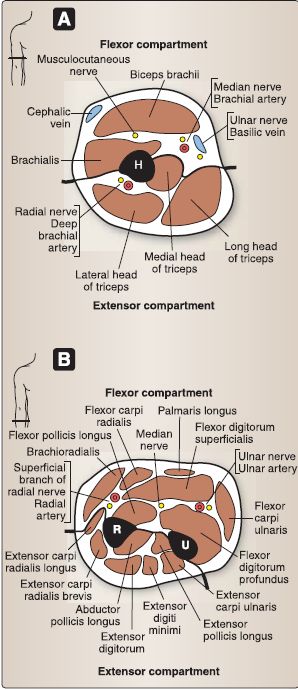
Figure 2: Cross-sectional anatomy of the upper limb. A, Arm. B, Forearm. H = humerus, R = radius, U = ulna.
2. Forearm and hand fascia: Distally, the brachial fascia continues into the forearm as the antebrachial fascia, also arranged in anterior and posterior compartments. At the wrist, the antebrachial fascia thickens into an anterior flexor retinaculum and posterior
extensor retinaculum, which function to maintain tendon position at the wrist. The fascia of the palm thickens into the palmar aponeurosis, which further compartmentalizes the hand.
C. Venous drainage
Venous drainage of the upper limb occurs through a superficial and deep venous network (Fig. 3).
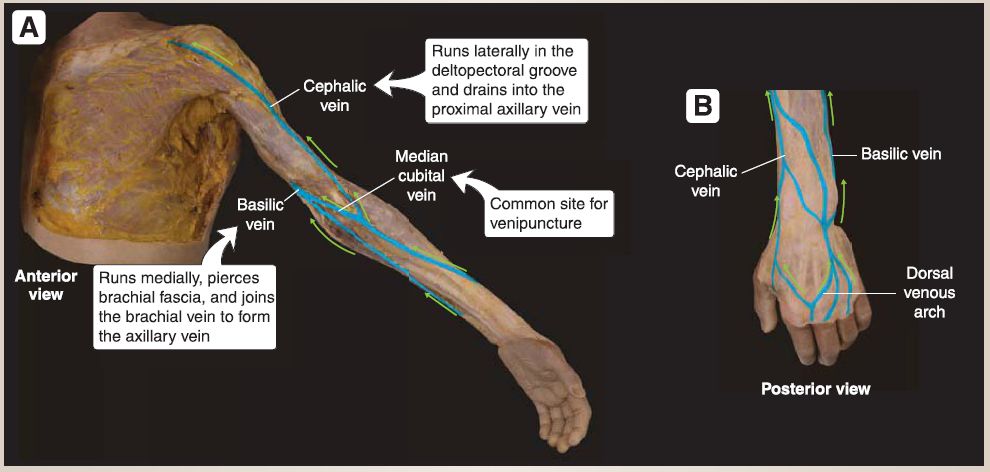 Figure 3: Superficial veins. A, Upper limb superficial vein network. B, Dorsum of hand venous network. Green arrows indicate direction of blood flow.
Figure 3: Superficial veins. A, Upper limb superficial vein network. B, Dorsum of hand venous network. Green arrows indicate direction of blood flow.
1. Superficial network: Superficially, the cephalic vein and basilic vein travel superiorly from the dorsum of the hand to drain into the axillary vein. The cephalic vein travels laterally and the basilic medially. Multiple, small tributary veins drain into these two main superficial veins, and they are connected at the cubital fossa by the median cubital vein.
a. Cephalic vein: The cephalic vein travels along the lateral forearm and arm and within the deltopectoral groove before piercing the costocoracoid membrane and clavipectoral fascia to drain into the proximal portion of the axillary vein.
b. Basilic vein: The basilic vein travels along the medial forearm and pierces the brachia! fascia midway along the arm to join the brachia! vein. The merging of the basilic and brachial veins forms the axillary vein.
c. Perforating veins: Multiple perforating veins pierce the deep fascia of the upper limb along the course of the superficial veins to connect superficial to deep veins. Both superficial and perforating veins have valves to ensure-under normal conditions- unidirectional blood return toward the heart.
2. Deep network: Deep veins of the upper limb travel with all major upper limb arteries and branches and typically carry the same name .
D. Lymphatics
Lymphatics of the upper limb are closely associated with the venous system (Fig. 4 ).
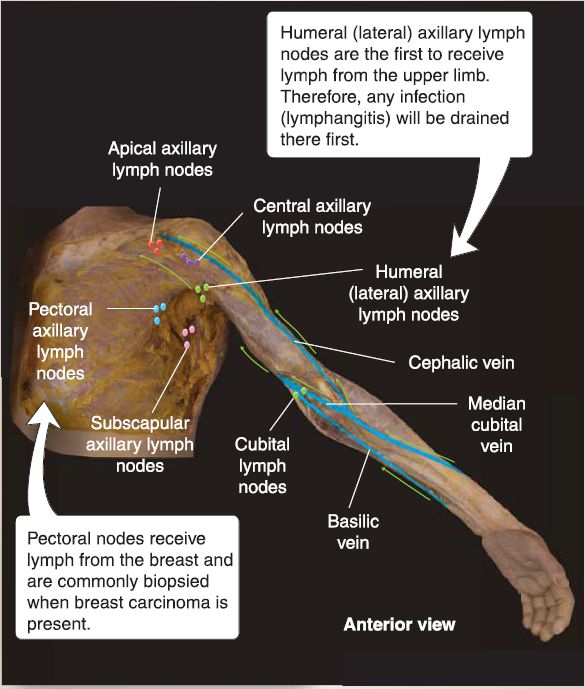
Figure 4: Lymphatics of the upper limb. Green arrows indicate direction of lymph flow.
1. Superficial lymphatic vessels: These travel with the cephalic andbasilic veins and drain into associated lymph nodes. Lymphatics that travel with the cephalic vein primarily drain into apical axillarylymph nodes first before being drained by the subclavian lymphatic trunk. Those that travel with the basilic vein partially drain into the cubital nodes located just superior to the medial epicondyle. From the cubital nodes, efferent lymph vessels travel to the humeral axillary nodes along deep veins.
2. Deep lymphatic vessels: These travel with deep veins in the upper limb, which first drain into humeral axillary nodes, then central axillary nodes, and finally apical axillary nodes, before being drained by the subclavian lymphatic trunk. Pectoral and subscapular axillary lymph nodes drain those respective regions of the upper limb.
E. Arterial supply
Upper limb structures receive arterial blood supply from branches of the subclavian, axillary, brachia!, ulnar, and radial arteries (Fig. 5).
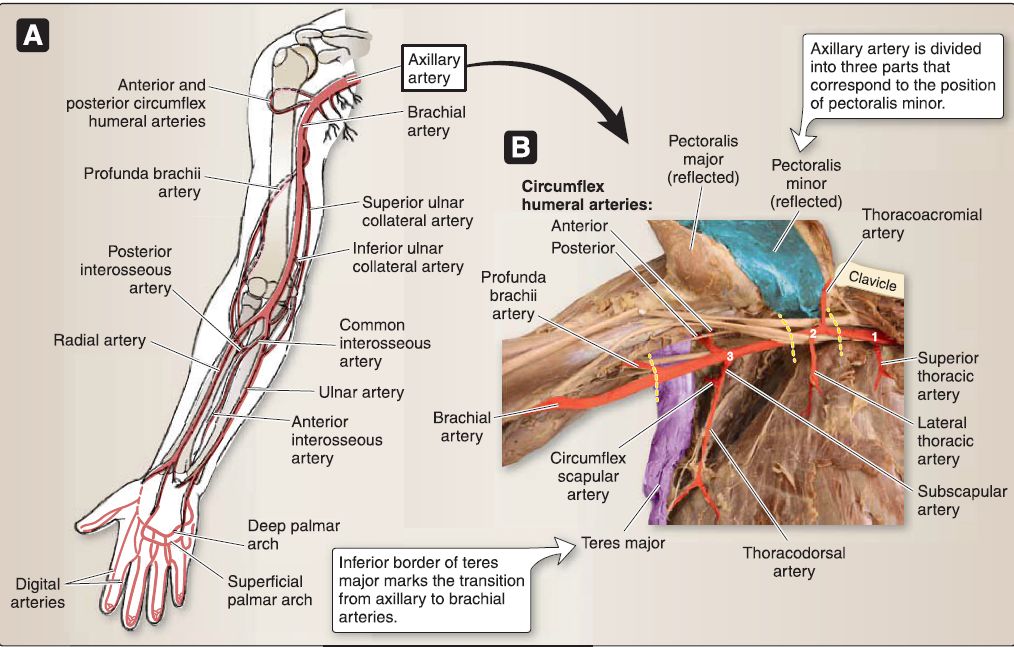
Figure 5: Arterial supply. A, Axillary artery through palmar arches. B, Dissection of axillary artery and branches (brachial plexus terminal nerves reflected). Numbers correspond to the three different parts of the axillary artery.
1. Subclavian artery: This artery sends branches to posterior axioappendicular muscles, which also contribute to collateral flow around the scapula. Branches include transverse cervical (to trapezius), dorsal scapular (to rhomboid major/minor and levator scapulae), and suprascapular (to supraspinatus and infraspinatus) arteries.
2. Axillary artery: After passing the lateral border of the first rib, the subclavian artery continues as the axillary artery. It is divided into three parts that correspond to the position of the pectoralis minor muscle.
a. First part: This part lies between the lateral border of the first rib and the medial border of pectoralis minor and gives off one branch-superior thoracic artery-to the second intercostal space.
b. Second part: This part lies deep to the pectoralis minor and gives off two branches-thoracoacromial and lateral thoracic arteries. The thoracoacromial artery gives off clavicular, pectoral, deltoid, and acromial branches that serve those respective structures. The lateral thoracic supplies the lateral pectoral region and serratus anterior muscle.
c. Third part: This part lies between the lateral border of pectoralis minor and the inferior border of teres major and gives off three branches-anterior and posterior circumflex humeral and subscapular arteries. The circumflex humeral arteries anastomose around the surgical neck of the humerus. The subscapular artery further divides into circumflex scapular and thoracodorsal arteries.
3. Brachia! artery: After crossing the inferior border of the teres major, the axillary artery continues as the brachia! artery. It supplies structures in the anterior arm and gives off a profunda brachii artery to serve the posterior arm structures. Superior and inferior ulnar collateral arteries arise from the brachia! artery medially and travel posterior and anterior to the medial epicondyle, respectively, to contribute to the collateral blood flow of the elbow.
4. Radial and ulnar arteries: In the cubital fossa, the brachia! artery divides into radial and ulnar arteries, which travel along the lateral and medial forearm, respectively. Just distal to its origin, the radial artery gives off a recurrent radial artery, which travels proximally to anastomose around the lateral elbow with collateral branches of the profunda brachii artery. The ulnar artery quickly gives off a common interosseous artery, which divides into anterior and posterior interosseous arteries. These travel deep along the interosseous membrane in their respective compartments to supply deep structures.
a. Palmar arterial arches: At the wrist, the ulnar and radial arteries contribute to palmar arterial arches. The ulnar artery primarily makes up the superficial palmar arch, while the radial artery contributes mainly to the deep palmar arch. Both arteries anastomose to complete the superficial and deep palmar arches.
b. Digital supply: The radial artery also gives off the princeps pollicis and radialis indicis arteries to the first and second digits, respectively. Common palmar digital arteries arise from the superficial palmar arch and give rise to proper palmar digital arteries in the digits. Dorsal digital arteries arise from the dorsal carpal arch.
F. Innervation
Upper limb structures are innervated by branches of the brachia! plexus, a collection of anterior primary rami from C5-C8 and T1 (Fig. 6).
 Figure 6: Brachia! plexus organization. A, In situ. Note rami and trunks in posterior triangle of neck, divisions running deep to clavicle, and chords and terminal branches in axilla. B, Schematic representation of right brachia! plexus from rami to terminal nerves.
Figure 6: Brachia! plexus organization. A, In situ. Note rami and trunks in posterior triangle of neck, divisions running deep to clavicle, and chords and terminal branches in axilla. B, Schematic representation of right brachia! plexus from rami to terminal nerves.
1. Brachial plexus: The brachia! plexus is divided into five parts from proximal to distal-rami, trunks (upper, middle, and lower), divisions (anterior and posterior), cords (lateral, medial, and posterior), and terminal branches. Small branches arise from rami, trunks, and cords. Cords and branches are contained within the axilla.
a. Rami (C5-C8, T1): Anterior rami branch from spinal nerves exiting the vertebral column in the neck and emerge between the anterior and middle scalene muscles. The dorsal scapular (C5) nerve arises from Cs anterior rambus.
b. Trunks: In the posterior triangle of the neck, anterior rami from C5-C6 merge to form the upper trunk, C7 continues as the middle trunk, and C8 and T1 merge to form the lower trunk. The nerve to subclavius (C5-C6) and the suprascapular (C5-C6) nerve arise from the upper trunk.
c. Divisions: Trunks divide into anterior and posterior divisions that serve pre- and postaxial structures, respectively. Divisions are found deep to the clavicle and have no branches.
d. Cords: Anterior divisions from the upper and middle trunks join to form the lateral cord. Posterior divisions from all trunks join to form the posterior cord. The anterior division from the lower trunk continues as the medial cord. Cords are named by their
relationship with the axillary artery.
[1] Lateral cord: This gives off the lateral pectoral nerve (C5-C7). [2] Medial cord: This gives off the medial pectoral (C8- T1), medial brachia! cutaneous (C8-T1), and medial antebrachial cutaneous (C8-T1) nerves.
[3] Posterior cord: This gives off upper subscapular (C5-C6), thoracodorsal (middle subscapular, C6-C8), and lower subscapular (C5-C6) nerves.
e. Terminal branches: Each cord terminates in two terminal branches. The median nerve (C5-C8, T1) is made up of the lateral and medial roots (Fig. 7 ).
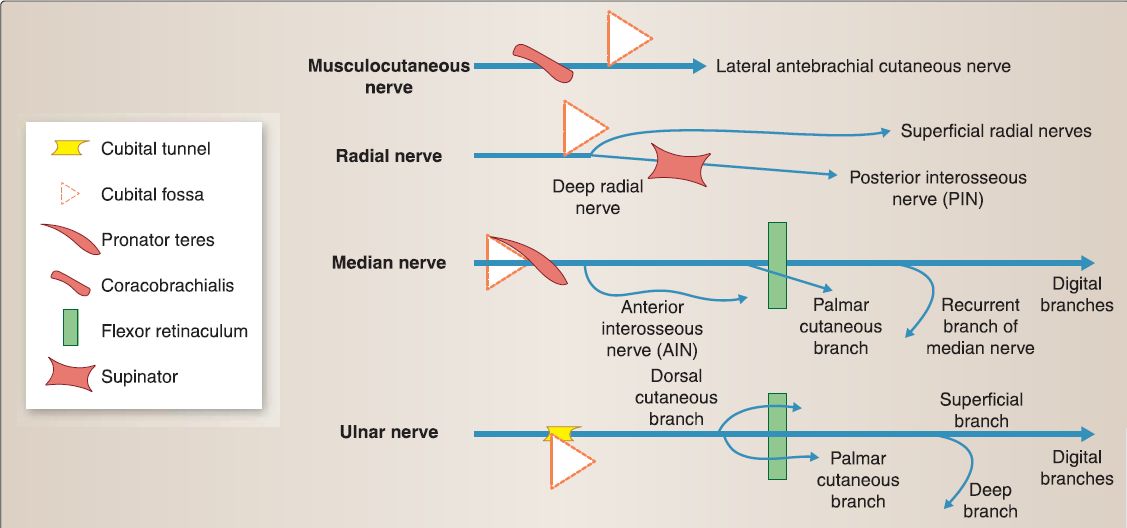
Figure 7: Terminal nerve distribution. Schematic drawings of terminal nerve pathway and branches {blue lines) and relationship between adjacent osseous, fascial, and muscular structures.
[1] Lateral cord: This divides into the lateral root of the median nerve and musculocutaneous nerve (C5-C7).
[2] Medial cord: This divides into the medial root of the medial nerve and ulnar nerve (C8-T1).
[3] Posterior cord: This divides into axillary (C5-C6) and radial (C5-C8, T1) nerves.
2. Cutaneous innervation: Cutaneous innervation of the upper limb is relayed primarily through branches of the brachia! plexus terminal nerves as well as supraclavicular (C3-C4) and intercostobrachial (T2) nerves (Fig. 8). Postganglionic sympathetic fibers travel with branches to provide general visceral afferent and general visceral efferent innervation to upper limb structures. Parasympathetic fibers do not travel in the upper limb.

Figure 8: Cutaneous distribution in the upper limb.
 الاكثر قراءة في علم التشريح
الاكثر قراءة في علم التشريح
 اخر الاخبار
اخر الاخبار
اخبار العتبة العباسية المقدسة

الآخبار الصحية










 قسم الشؤون الفكرية يصدر كتاباً يوثق تاريخ السدانة في العتبة العباسية المقدسة
قسم الشؤون الفكرية يصدر كتاباً يوثق تاريخ السدانة في العتبة العباسية المقدسة "المهمة".. إصدار قصصي يوثّق القصص الفائزة في مسابقة فتوى الدفاع المقدسة للقصة القصيرة
"المهمة".. إصدار قصصي يوثّق القصص الفائزة في مسابقة فتوى الدفاع المقدسة للقصة القصيرة (نوافذ).. إصدار أدبي يوثق القصص الفائزة في مسابقة الإمام العسكري (عليه السلام)
(نوافذ).. إصدار أدبي يوثق القصص الفائزة في مسابقة الإمام العسكري (عليه السلام)