Ear
The ear is the organ of balance and hearing. What we commonly call the "ear" actually consists of the three components: an internal ear, a middle ear, and an external ear.
A. Internal ear
The internal ear is found in the petrous temporal bone and houses the specialized organs of balance (vestibular system) and hearing (auditory system).
1. Embryology: At week 4, the internal ear develops from a thickening of the surface ectoderm called the otic placode (Fig. 1). The otic placode invaginates into the underlying mesenchyme adjacent to the rhombencephalon and becomes the otic vesicle. The otic vesicle divides into an upper utricular portion and a lower saccular portion.
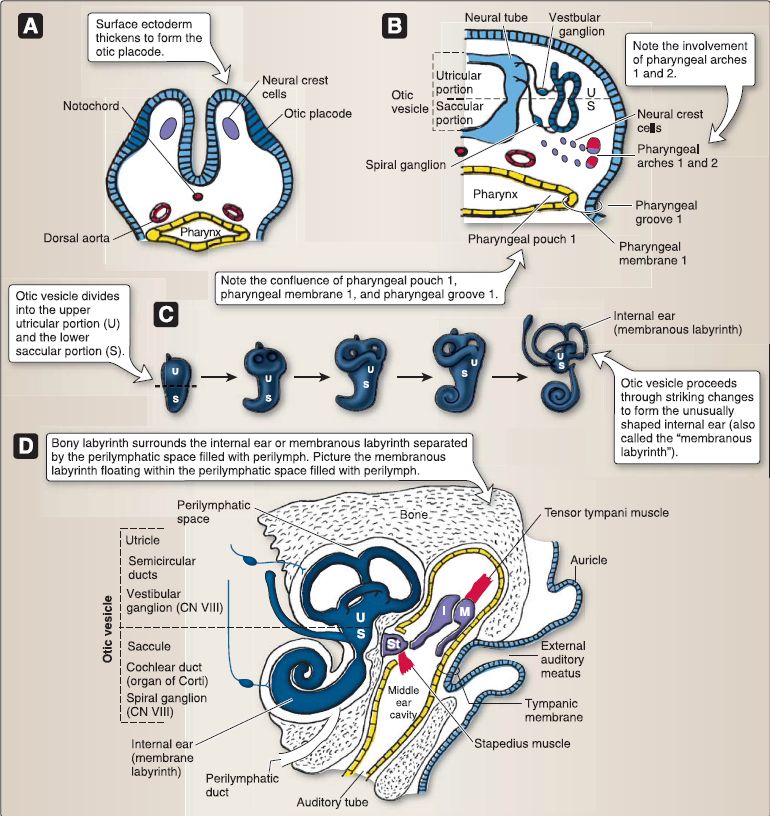
Figure 1: Internal, middle, and external ear development (A-D). I = incus, M = malleus, ST = stapes.
a. Utricular portion: The upper portion of the otic vesicle gives rise to the following.
[1] Utricle: This structure contains the sensory hair cells and otoliths located in a specific region called the macula of the utricle. The utricle responds to linear acceleration and the force of gravity.
[2] Semicircular ducts: These contain the sensory hair cells of the cristae ampullares. The semicircular ducts respond to angular acceleration.
[3] Vestibular ganglion of CN VIII: This lies at the base of the internal auditory meatus.
[4] Endolymphatic duct and sac: This membranous duct connects the saccule to the utricle and terminates in a blind sac beneath the dura. The endolymphatic sac is involved in fluid exchange.
b. Saccular portion: The lower portion of the otic vesicle gives rise to the following.
[1] Saccule: This structure contains the sensory hair cells and otoliths located in a specific region called the macula of the saccule. The saccule responds to linear acceleration and the force of gravity.
[2] Cochlear duct (organ of Corti): Involved in hearing, this duct has pitch (tonopic) localization whereby high-frequency sound waves (20,000 Hz) are detected at the base, and lowfrequency sound waves (20 Hz) are detected at the apex.
[3] Spiral ganglion of CN VIII: This lies in the modiolus of the bony labyrinth.
c. Membranous labyrinth: At week 8, the utricular and saccular portions of the otic vesicle have formed the abovementioned structures, sometimes collectively referred to as the membranous labyrinth. The terms "membranous labyrinth" and "bony labyrinth" cause much confusion, but an understanding of them is crucial in order to appreciate the anatomical and physiologic functions of the internal ear.
[1] Endolymph: The soft, cellular membranous labyrinth is filled with endolymph and consists of all the ectodermal structures derived from the utricular portion and the saccular portion of the otic vesicle. The endolymph is similar to intracellular fluid and is exchanged using the endolymphatic duct and sac. The membranous labyrinth is completely surrounded by neural crest cells that form a connective tissue covering. This connective tissue becomes cartilaginous and then ossifies to become the bony labyrinth of the temporal bone.
[2] Perilymph: However, the connective tissue directly opposed to the membranous labyrinth degenerates, thus forming the perilymphatic space filled with perilymph that lies between the membranous labyrinth and the bony labyrinth. This establishes an interesting anatomical relationship in which the membranous labyrinth filled with endolymph floats within the bony labyrinth filled with perilymph. The perilymph is similar to CSF and communicates with the subarachnoid space via the perilymphatic duct.
2. Histology: The internal ear (or the membranous labyrinth) is composed of two divisions: vestibular and cochlear labyrinths. The vestibular labyrinth consists of the semicircular ducts, the utricle, and the saccule. The cochlear labyrinth consists of the cochlear duct. Chaliceshaped
a. Vestibular labyrinth: The three semicircular ducts (i.e., anterior, posterior, and horizontal) each have a swelling at one end where it joins the utricle called the ampulla (Fig. 2). On the floor of each ampulla rests an ampullary crest.
 Figure 2: Vestibular labyrinth histology. A, Location of ampullary crests (red) within the ampulla {blue) at the base of each semicircular duct. B, Light micrograph of the left boxed area in C (arrow). C, Light micrograph showing the ampullary crest on the floor of the ampulla {filled with endolymph) and its relationship to the cupula as well as the macula of the utricle on the floor of the utricle {filled with endolymph). D, Location of the macula of the utricle (red) and macula of the saccule (red) within two swellings called the utricle (blue) and saccule (blue). E, Light micrograph of the right boxed area in C (arrow). The macula of the utricle consists of a connective tissue base covered by hair cells and support cells. F, Morphology of types I and II hair cells and their relationship to afferent and efferent nerve fibers.
Figure 2: Vestibular labyrinth histology. A, Location of ampullary crests (red) within the ampulla {blue) at the base of each semicircular duct. B, Light micrograph of the left boxed area in C (arrow). C, Light micrograph showing the ampullary crest on the floor of the ampulla {filled with endolymph) and its relationship to the cupula as well as the macula of the utricle on the floor of the utricle {filled with endolymph). D, Location of the macula of the utricle (red) and macula of the saccule (red) within two swellings called the utricle (blue) and saccule (blue). E, Light micrograph of the right boxed area in C (arrow). The macula of the utricle consists of a connective tissue base covered by hair cells and support cells. F, Morphology of types I and II hair cells and their relationship to afferent and efferent nerve fibers.
[1] Ampullary crest: The ampullary crest is an elevated ridge of connective tissue covered by an epithelium and the cupula. The epithelium consists of type I hair cells, type II hair cells, and support cells. The cupula is a gelatinous mass that covers the epithelium and extends to the roof of the ampulla.
(a) Type I hair cell: Pear shaped with a basally located nucleus, the type I hair cell forms a single, chalice-like synapse with bipolar afferent neurons from the vestibular ganglion of CN VIII. Efferent neurons are also present that set the sensitivity of the type I hair cell. The type I hair cell has a single kinocilium and 40-100 stereocilia of varying lengths embedded in the cupula.
(b) Type II hair cell: Cylinder shaped with a centrally located nucleus, the type II hair cells form multiple, small, bouton-like synapses with bipolar afferent neurons from the vestibular ganglion of CN VIII. Efferent neurons are also present that set the sensitivity of the type II hair cell. The type II hair cell has a single kinocilium and 40-100 stereocilia of varying lengths embedded in the cupula.
(c) Support cells: These rest on the basal lamina and provide support by cradling the hair cells. The semicircular ducts respond to rotational (angular) acceleration or deceleration of the head. Head rotation drags the cupula through the endolymph, causing the cupula to bend, thereby deflecting hair cell stereocilia. When stereocilia are deflected toward the kinocilium, action potential discharge increases (depolarization). When stereocilia are deflected away from the kinocilium, action potential discharge decreases (repolarization).
[2] Macula: On the floor of both the utricle and saccule rests a region of specialized epithelium called the macula (i.e., macula of the utricle and macule of the saccule), as shown in Figure 2. The histology of the macula of the utricle and that of the macula of the saccule is the same. The macula is a region of connective tissue covered by an epithelium, the otolithic membrane, and otoconia. The epithelium consists of the same types I and II hair cells and support cells as those of the ampullary crest (see above). The otolithic membrane is a gelatinous mass that covers the epithelium. The otoconia are tiny calcium carbonate (CaC03) crystals that are attached to the surface of the otolithic membrane.
b. Cochlear labyrinth: The cochlear duct is a triangle-shaped duct that is coiled -2. 75 times, much like the tail of a snail (Fig. 3). The cochlear duct is suspended across the bony labyrinth, so that the space above the cochlear duct is the scala vestibuli and filled with perilymph, and the space below the cochlear duct is the scala tympani and also filled with perilymph. The lumen of the cochlear duct is called the scala media, which contains endolymph.
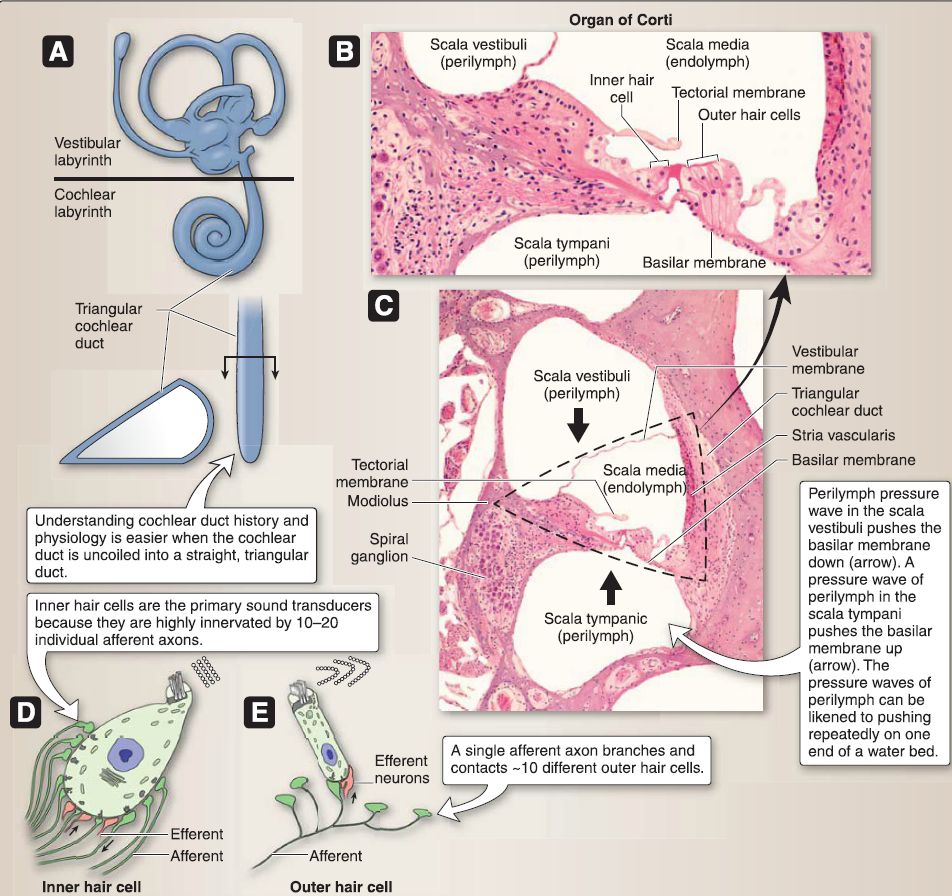 Figure 3: Cochlear labyrinth histology (A-E).
Figure 3: Cochlear labyrinth histology (A-E).
[1] Boundaries: The boundaries of the cochlear duct are the vestibular membrane that forms the roof, the basilar membrane that forms the floor, the stria vascularis that forms the lateral wall, and the bony modiolus that forms the medial wall.
[2] Stria vascularis: The stria vascularis is a highly vascularized stratified epithelium that produces the endolymph and maintains the high K+ concentration in the endolymph.
[3] Organ of Corti: The organ of Corti rests on the basilar membrane and is a band of connective tissue covered by an epithelium and the tectorial membrane, a gelatinous mass that covers the epithelium and extends to the spiral limbus. The epithelium consists of a single row of 3,500 inner hair cells, three rows of 20,000 outer hair cells, and a number of different types of supporting cells (i.e., border cells, phalangeal cells, pillar cells, cells of Boettcher, and cells of Claudius).
(a) Inner hair cell: Pear shaped with a basally located nucleus that is completely surrounded by inner phalangeal cells, the inner hair cell forms multiple synapses with bipolar afferent neurons from the spiral ganglion of CN VIII. Efferent neurons are also present that set its sensitivity. The inner hair cell lacks a kinocilium but has 40-100 stereocilia of varying lengths arranged in a straight line and embedded in the tectorial membrane.
(b) Outer hair cell: Cylinder shaped with a centrally located nucleus that is only partially surrounded by outer phalangeal cells, the outer hair cell forms multiple synapses with bipolar afferent neurons from the spiral ganglion of CN VIII. Efferent neurons are also present that set its sensitivity. The outer hair cell lacks a kinocilium but has 40-100 stereocilia of varying lengths arranged in a V-shaped pattern and embedded in the tectorial membrane.
[4] Function: The cochlear duct responds to sound. The motion of the stapes at the oval window sets up a pressure wave in the perilymph within the scala vestibuli. This pressure wave travels down the scala vestibuli, through the helicotrema at the apex, and then back up the scala tympani to the round window. The pressure wave in the scala vestibuli pushes the basilar membrane of the organ of Corti down, thereby deflecting hair cell stereocilia away from the tallest length. When the stereocilia are deflected away from the tallest length, action potential discharge decreases. The pressure wave in the scala tympani pushes the basilar membrane of the organ of Corti up, thereby deflecting stereocilia toward the tallest length. When stereocilia are deflected toward the tallest length, action potential discharge increases.
3. Anatomy: The internal ear cavity lies deep within the otic capsule of the petrous temporal bone and houses the vestibulocochlear organ complex (Fig. 4). The bony and membranous labyrinths are contained within the otic capsule. The components of the vestibular complex include the semicircular canals, semicircular ducts, vestibule, utricle, and saccule. The vestibular complex is located posterosuperior to the cochlear complex. The cochlear complex consists of the cochlea, cochlear duct, scala tympani, and scala vestibuli, as previously described.
 Figure 4: Ear anatomy.
Figure 4: Ear anatomy.
The vestibulocochlear nerve (CN VIII) passes from the pons through the internal acoustic meatus to provide special sensory (SS) innervation to these structures (outlined above).
B. Middle ear
The middle ear houses the ear ossicles that function to transfer sound waves into mechanical energy for interpretation of sounds.
1. Embryology: At week 4, the middle ear begins to develop from a number of different sources: pharyngeal arch 1, pharyngeal arch 2, pharyngeal pouch 1, and pharyngeal membrane 1 .
a. Ossicles: The ossicles of the middle ear include the malleus, incus, and stapes.
[1] Malleus: The malleus develops from Meckel's cartilage derived from neural crest cells within pharyngeal arch 1. It is attached to the tympanic membrane and is moved by the tensor tympani muscle derived from mesoderm within pharyngeal arch 1. The tensor tympani muscle is innervated by CN V3 and functions to dampen loud sounds.
[2] lncus: The incus develops from Meckel's cartilage derived from neural crest cells within pharyngeal arch 1. The incus articulates with the malleus and stapes.
[3] Stapes: The stapes develops from Reichert's cartilage derived from neural crest cells within pharyngeal arch 2. The stapes is attached to the oval window of the vestibule and is moved by the stapedius muscle derived from mesoderm within pharyngeal arch 2. The stapedius muscle is innervated by CN VII and functions to dampen loud sounds.
b. Epithelial linings: The epithelial lining of the auditory tube and epithelial lining of the middle ear cavity develop from endoderm of pharyngeal pouch 1 .
c. Tympanic membrane: The tympanic membrane develops from ectoderm, intervening mesoderm and neural crest cells, and endoderm of pharyngeal membrane 1. The tympanic
membrane separates the middle ear from the external auditory meatus of the external ear. The tympanic membrane receives general visceral afferent (GVA) innervation internally by the tympanic plexus of the glossopharyngeal (CN IX) nerve.
2. Anatomy: The air-filled middle ear cavity is housed within the petrous temporal bone, deep to the tegmen tympani (Fig. 5). a. Walls: The lateral (membranous) wall of this cavity is associated with the tympanic membrane, the medial (labyrinthine) wall with the promontory and oval window with the stapes base, the roof (tegmental wall) with the tegmen tympani of the temporal bone, the floor Gugular wall) with the temporal bone adjacent to the jugular foramen, the posterior (mastoid) wall with the aditus (opening to mastoid air cells), and the anterior (carotid) wall with the auditory (pharyngotympanic) tube.
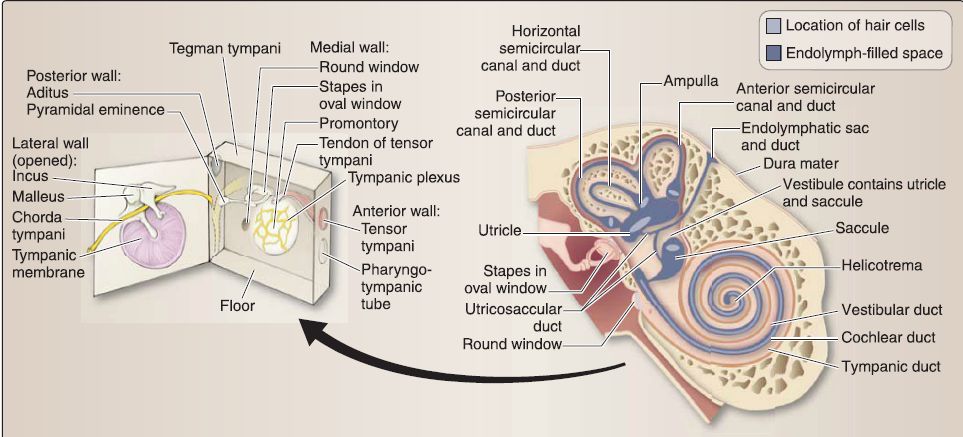 Figure 5: Middle and inner ear anatomy. Note boundaries and associated structures in middle ear (black arrow).
Figure 5: Middle and inner ear anatomy. Note boundaries and associated structures in middle ear (black arrow).
b. Contents: Auditory ossicles are housed within the middle ear, forming a kinetic chain that propagates vibrations from the external environment to the internal ear for processing. Both the stapedius and tensor tympani muscles function to dampen loud sounds by limiting the oscillation of the stapes and malleus. Both muscles extend into the middle ear cavity to insert onto their respective bones. The middle ear cavity also houses portions of two CNs-chorda tympani nerve (branch from the facial nerve) and the tympanic plexus (from the glossopharyngeal nerve). The chorda tympani nerve passes through the middle ear cavity en route to the infratemporal fossa. The tympanic plexus provides GVA innervation to the middle ear cavity before exiting as the lesser petrosal nerve.
C. External ear
The external ear is represented externally as a semirigid structure that is designed to funnel sounds wave toward the middle ear.
1. Embryology: At week 4, the external ear begins to develop from a number of different sources: pharyngeal groove 1 , pharyngeal arch 1, and pharyngeal arch 2 .
a. Auditory meatus: The epithelial lining of the external auditory meatus develops from ectoderm of pharyngeal groove 1. The external auditory meatus becomes filled with ectodermal cells that form a temporary meatal plug that disappears before birth. The external auditory meatus is innervated by CNs V3 and IX.
b. Auricle: The auricle develops from six auricular hillocks that form as six mesenchymal proliferations associated with pharyngeal arches 1 and 2. The six auricular hillocks surround pharyngeal groove 1. The auricle is innervated by CNs V3, VII, IX, and X and cervical nerves C2 and C3•
2. Anatomy: The external ear is characterized externally by the auricle (pinna), which contains an elastic cartilage core and overlying skin (Fig. 6).

Figure 6: External ear anatomy.
a. Auricle: The auricular cartilage imparts the shape of the external ear. It functions to funnel sounds in to the external acoustic canal toward the middle ear cavity. Features of the auricle are described below.
[1] Helix: This is the elevated outer rim of the auricle.
[2] Antihelix: This is the rounded projection adjacent to the helix.
[3] Concha: This is the deepest depression and is bound by the helix and antihelix.
[4] Tragus: This process overlaps the opening of the external acoustic meatus.
[5] Antitragus: This process lies opposite the tragus.
[6] Lobule: This is the ear lobe absent cartilage.
b. External acoustic canal: The external acoustic canal is one-third cartilaginous distally and two-thirds bony toward the middle ear cavity. Although typically straight during development, the canal assumes an "S" shape in adulthood. A mixture of sebaceous and apocrine glands line the outer third of the canal and collectively produce cerumen (ear wax) to lubricate and protect the skin in this region. Skin in the inner portion of the canal typically does not contain hair follicles or glands .
[1] Innervation: The canal receives sensory (GSA) innervation from the auriculotemporal branch (CN IX) and auricular branches (CN X). These branches also supply sensory innervation to the outer surface of the tympanic membrane,in addition to the posterior auricular branch of the facial nerve (CN VII).
[2] Lymphatics: Lymphatic drainage from the external ear occurs either through parotid (anterior superior), mastoid (posterior superior), or superficial cervical (inferior) nodes associated with the external jugular vein.
 الاكثر قراءة في علم التشريح
الاكثر قراءة في علم التشريح
 اخر الاخبار
اخر الاخبار
اخبار العتبة العباسية المقدسة


