Orbit
The orbits are paired pyramid-shaped cavities that house the eyeballs and associated muscular, neuromuscular, glandular, and connective tissue structures (Fig. 1). Each orbit is angled such that the apex faces posteromedially and the base anterolaterally. The apex is located at the optic canal and the base at the orbital rim.

Figure 1: Bony orbit.
A. Osteology
A number of neurocranial and viscerocranial bones contribute to the formation of the bony orbit. A periosteal layer called the periorbita lines the bones that form the orbit and is continuous posteriorly with periosteal dura, anteriorly with the pericranium, and internally with the extraocular muscle and orbital fasciae. For descriptive purposes, the orbit is divided into superior (roof), inferior (floor), medial, and lateral walls.
1. Superior wall: The frontal bone (orbital portion) and sphenoid (lesser wing) contribute superiorly.
2. Inferior wall: The maxilla and zygomatic bones contribute inferiorly, with the palatine bone also making a small contribution.
3. Medial wall: Frontal, ethmoid, lacrimal, and sphenoid bones contribute medially.
4. Lateral wall: Zygomatic (frontal process) and sphenoid (greater wing) bones contribute laterally.
B. Eyelids and lacrimal apparatus
Collectively, upper and lower eyelids function to protect the anterior surface of the eyeball and aid in corneal lubrication (Fig. 2). Eyelids possess an outer thin layer of skin and an inner mucous membrane, the palpebral conjunctiva. The substance between these two layers includes muscle fibers from orbicularis oculi (palpebral portion) superficially and extensions of levator palpebrae superioris (upper eyelid only).
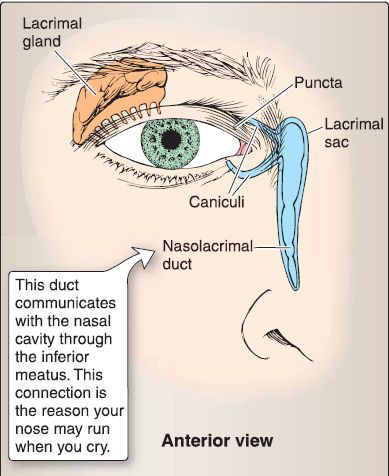
Figure 2: Lacrimal apparatus.
1. Eyelid: Deep to the muscle fibers, each eyelid is supported by superior and inferior plates of connective tissue, called tarsi (singular = tarsus). Tarsal glands are dispersed within each tarsus. These glands produce a lipid-rich secretion that functions to lubricate the eyelid's free edge and form a boundary for lacrimal fluid. Medial and lateral tarsal ligaments extend from the tarsi to support the eyelids and connect them to the medial and lateral orbital walls, respectively. A broad orbital septum completes the connection to the orbital margin. Eyelashes extend from the free edge of each eyelid and are associated with sebaceous ciliary glands.
2. Conjunctiva! sac: The space between the palpebral conjunctiva surface of the eyelids and the bulbar conjunctiva of the eyeball is called the conjunctiva! sac. Superior and inferior conjunctiva! fornices serve as superior and inferior limits of this specialized bursa-like space, thus allowing for free movement of the eyelids on the eyeball.
3. Lacrimal apparatus: The lacrimal apparatus is structurally and functionally related to the eyelid and eyeball.
a. Lacrimal gland: The small lacrimal gland sits in the superolateral wall of the orbit, in a depression called the lacrimal fossa. It produces lacrimal fluid, which is secreted to the surface of the eyeball through a series of 8-12 ducts. Stimulation of fluid production is under autonomic control through parasympathetic fibers from the facial nerve (CN VII).
b. Lacrimal sac: Aided by gravity and the blinking motion of the eyelids, fluid spreads across the cornea in a lateral-to-medial direction toward the lacrimal lake at the medial angle of the eyelids. Fluid is taken up through lacrimal caruncles and deposited into the lacrimal sac. The lacrimal sac is a thin-walled structure that sits in a depression in the lacrimal bone along the medial wall of the orbit. Inferiorly, the sac communicates with the nasolacrimal duct, which serves as a conduit to transport lacrimal fluid from the sac to the nasal cavity and, eventually, the nasopharynx.
C. Eye
Understanding how the eye develops is critical to understanding its anatomy. In the developing eye, an optic cup of neuroectoderm is surrounded by an embryonic connective tissue called mesenchyme. The question is, What does this mesenchyme become? The answer is that the mesenchyme directly around the optic cup forms a vascular tunic called the choroid, and the outermost mesenchyme forms a fibrous tunic called the sclera. Consequently, the general feature of the adult eye is that it consists of three concentric tunics: the innermost tunic (optic cup; neuroectoderm), middle tunic {choroid; mesenchyme), and the outermost tunic (sclera; mesenchyme).
1. Embryology: At day 22, the eye begins to develop when the neural plate in the forebrain region (i.e., the future diencephalon) begins to fold to form a closed neural tube.
a. Optic vesicle development: The neural plate (neuroectoderm) on each side indents to form the optic sulci (Fig. 3). Each optic sulcus expands from the forebrain to form the optic vesicle. The optic vesicle grows toward the surface ectoderm and induces the formation of the lens placode.
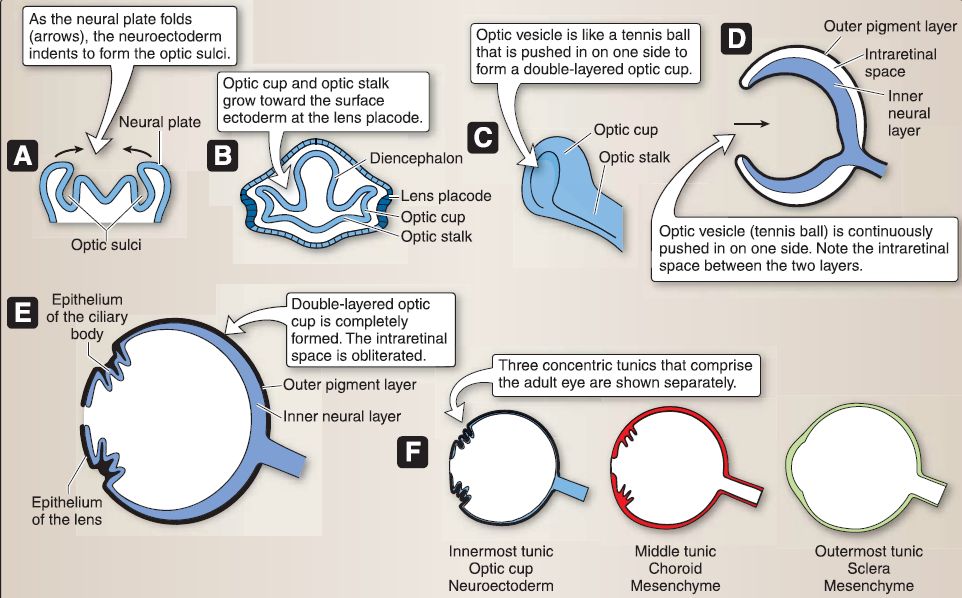 Figure 3: Optic vesicle development
Figure 3: Optic vesicle development
b. Optic cup development: At day 28, the optic vesicle invaginates to form a double-layered optic cup of neuroectoderm. The optic cup remains attached to the forebrain by the optic stalk. The double-layered optic cup consists of an outer pigment layer and an inner neural layer. The optic cup gives rise to the retina, the epithelium of the ciliary body, and the epithelium of the iris.
[1] Retina: The outer pigment layer of the optic cup gives rise to the outer pigment layer of the retina. The inner neural layer of the optic cup gives rise to the inner neural layer of the retina.
[2] Epithelium of the ciliary body: The epithelium of the ciliary body is unique in that it consists of two opposing layers of epithelium continuous with the outer pigment layer of the optic cup and the other continuous with the inner neural layer of the optic cup (Fig. 4).
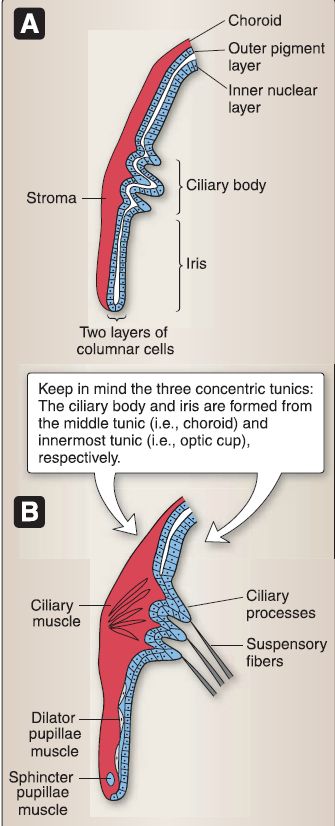
Figure 4:Ciliary body and iris development (A and B).
(a) Strama: The stroma of the ciliary body is derived from mesenchyme that is continuous with the choroid (i.e., the middle tunic).
(b) Ciliary muscle: The ciliary muscle is derived from mesenchyme continuous with the choroid.
[3] Epithelium of the iris: The epithelium of the iris is unique in that it consists of two opposing layers of epithelium continuous with the outer pigment layer of the optic cup and the other continuous with the inner neural layer of the optic cup.
(a) Strama: The stroma of the iris is derived from mesenchyme that is continuous with the choroid (i.e., the middle tunic).
(b) Muscles: The dilator pupillae muscle and sphincter pupillae muscle are formed from the epithelium of the outer pigment layer by a transformation of these epithelial cells into contractile cells.
c. Optic stalk development: At day 28, the ventral portion of the optic stalk invaginates to form the optic fissure (Fig. 5). The optic fissure contains the hyaloid artery and vein. The hyaloid artery supplies the developing retina and the developing lens vesicle. The fully mature lens ceases to need a blood supply, so the portion of the hyaloid artery that crosses the vitreous body degenerates and leaves a remnant called the hyaloid canal. At week 7, the optic fissure seals and entraps the hyaloid artery and vein, which later become the central artery and vein of the retina. As the inner neural layer continues to proliferate, the increasing number of axons from the ganglion cell layer of the retina obliterate the intraretinal space. The optic stalk forms the optic nerve (CN II), optic chiasm, and optic tract in the adult.
 Figure 5: Optic stalk development (A-C).
Figure 5: Optic stalk development (A-C).
d. Cornea development: The cornea develops from both surface ectoderm and mesenchyme that lies anterior to the anterior chamber and that is continuous with the sclera (i.e., the outermost tunic), as shown in Figure 6. The surface ectoderm forms upper and lower infoldings that eventually develop into the upper and lower eyelids (Recall that the space between the two layers of ectoderm is the conjunctiva! sac.). A portion of the surface ectoderm reflects over the mesenchyme that is continuous with the sclera. The surface ectoderm forms the anterior epithelium of the cornea, which has a high regenerative capacity. The mesenchyme forms the substantia propria of the cornea (i.e., Bowman layer, stroma, and Descemet membrane) and the corneal endothelium.
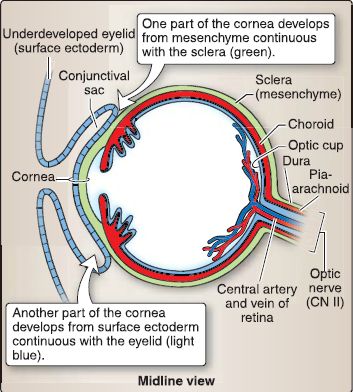
Figure 6: Cornea development.
e. Lens development: When the optic vesicle gets close to the surface ectoderm, the surface ectoderm in that vicinity thickens to form the lens placode (Fig. 7). The lens placode invaginates shortly thereafter to form the lens pit and then completely separates from the surface ectoderm to become the hollow lens vesicle surrounded by a lens capsule. At day 33, the cells on the posterior surface of the lens vesicle differentiate to form primary lens fibers that elongate to obliterate the lumen of the lens vesicle to form the lens body. The cells on the anterior surface of the lens vesicle remain mitotically active throughout life, migrate to the lens equator, and form the secondary lens fibers.
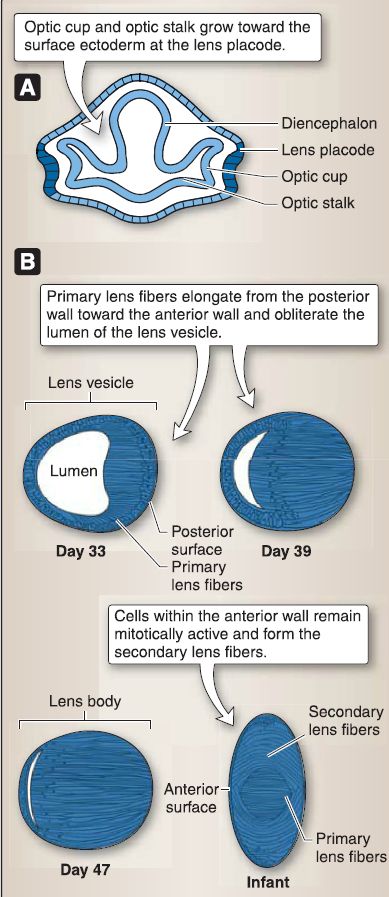
Figure 7: Lens development (A and B).
2. General histologic features of the eye: Recall that the eye comprises three concentric tunics (Fig. 8). The lens is suspended by zonular fibers (forming the suspensory ligament) that originate from the ciliary body. The posterior and anterior chambers of the eye are filled with aqueous humor, which is a clear, plasma-like fluid secreted by the epithelium of the ciliary body. The vitreous cavity is filled with the vitreous body, which is a transparent gelatinous substance that consists of water, some collagen fibers, and hyaluronan.
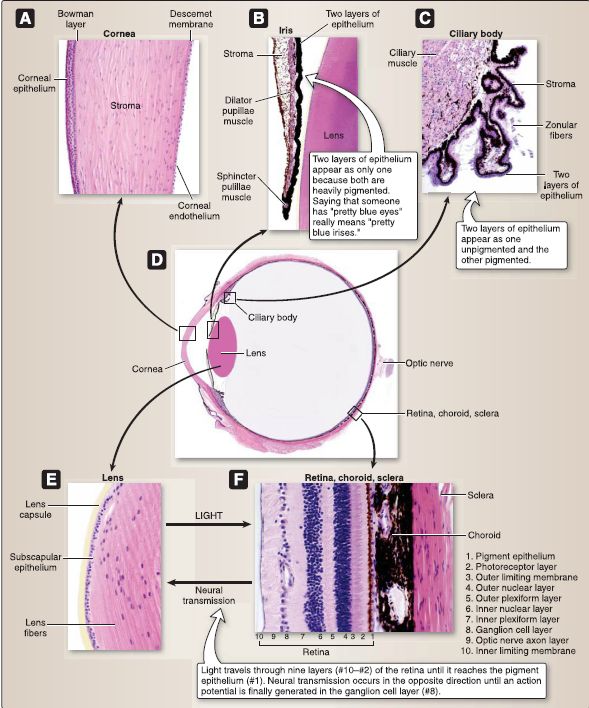
Figure 8: Eye histology (A-F).
a. Tunics: The adult eye wall contains the corneoscleral, uveal, and retinal tunics.
[1] Corneoscleral tunic: The outermost fibrous tunic consists of the white, opaque sclera and transparent cornea. Covering the posterior five-sixths of the eyeball, the sclera is a thick, opaque layer of collagen and elastic fibers produced by fibroblasts. The tendons of the extraocular muscles attach to the sclera. The corneoscleral junction (or limbus) is the junction of the transparent cornea and the opaque sclera.
[2] Uveal tunic: The middle vascular tunic consists of the choroid, the stroma of the ciliary body, and the stroma of the iris. The choroid is a connective tissue layer, between the sclera and retina, that contains fibroblasts, collagen fibers, elastic fibers, macrophages, lymphocytes, mast cells, plasma cells, and numerous melanocytes that give this layer its characteristic brown/black appearance. The inner portion of the choroid is highly vascularized and is called the choriocapillary layer.
[3] Retinal tunic: The innermost tunic consists of the pigment epithelium, the neural retina, the epithelium of the ciliary body, and the epithelium of the iris.
b. Cornea: Covering the anterior sixth of the eyeball, the cornea is an avascular, transparent structure composed of five layers: corneal and Bowman layers, stroma, Descemet membrane, and corneal endothelium.
[1] Corneal layer: The corneal epithelium is a nonkeratinized stratified squamous epithelium that covers the anterior surface of the cornea (i.e., the surface exposed to air). The cornea, more so than the lens, is responsible for retracing light, thus allowing for the focusing of an inverted image on the retinal fundus.
[2] Bowman layer: This layer is not considered a true basal lamina but is a distinctive portion of the corneal stroma that contains randomly arranged type I collagen fibers.
[3] Stroma: The stroma is the thickest layer of the cornea and consists of connective tissue composed of fibroblasts, ground substance, and types I and V collagen fibers. The stroma is orderly arranged in about 60 layers. The collagen fibrils in each layer are oriented perpendicular to the collagen fibrils in the adjacent layer.
[4] Descemet membrane: The Descemet membrane is the thick basal lamina that lies beneath the corneal endothelium.
[5] Corneal endothelium: This simple squamous epithelium covers the posterior surface of the cornea (i.e., the surface exposed to aqueous humor).
c. Ciliary body: Posterior to the corneoscleral junction sits the thickened, ringlike ciliary body, which serves as an attachment site for the lens. Folds of tissue, called the ciliary process, extend internally from the ciliary body. The ciliary body and ciliary processes consist of an epithelium and a stroma.
[1] Ciliary epithelium: This consists of two layers of simple columnar epithelium, only one of which is heavily pigmented by melanin. The two layers of simple columnar epithelium are continuous with the outer pigmented layer of the retina and the inner non pigmented neural layer of the retina. The inner, nonpigmented layer of the ciliary epithelium associated with the ciliary processes, secretes aqueous humor into the posterior chamber and produces the zonular fibers that attach to the lens capsule.
[2] Stroma: The highly vascularized stroma consists of fibroblasts, melanocytes, collagen fibers, and the ciliary muscle. The ciliary muscle functions in the process of accommodation, whereby the lens becomes flatter to focus on distant objects or rounder to focus on nearby objects.
d. Iris: The iris is located on the anterior surface of the lens. It consists of an epithelium and a stroma.
[1] Epithelium: The iris epithelium consists of two layers of simple columnar epithelium both of which are heavily pigmented by melanin. The two layers of simple columnar epithelium are continuous with the outer pigmented layer of the retina and the inner non pigmented neural layer of the retina.
[2] Stroma: The stroma of the iris forms an irregular surface with numerous grooves and ridges. The highly vascularized stroma consists of fibroblasts, melanocytes, collagen fibers, the dilator pupillae muscle, and the sphincter pupillae muscle. The dilator pupillae muscle is radially arranged around the entire circumference of the iris and is innervated by the sympathetic nervous system. The sphincter pupillae muscle is circularly arranged around the entire circumference of the iris and is innervated by the parasympathetic nervous system. Coordination of these muscles changes the diameter of the iris's aperture, the pupil, in response to light and other stimulation.
e. Lens: The lens is a biconvex, transparent, avascular structure located posterior to the iris. It consists of a lens capsule, a subcapsular epithelium, and lens fibers. The lens is attached to the ciliary processes by zonular fibers that constitute the suspensory ligament of the lens. For distance vision, ciliary muscles are relaxed, and the lens assumes a stretched, thin shape. For near vision, ciliary muscles contract, and the lens assumes a thicker, more spherical shape.
[1] Lens capsule: The lens capsule is a thick basal lamina containing type IV collagen that completely surrounds the lens.
[2] Subcapsular epithelium: This simple cuboidal epithelium is located beneath the lens capsule only on the anterior surface and at the equatorial region (i.e., no epithelium is found on the posterior surface). The subcapsular epithelium is mitotically active and migrates to the equatorial region of the lens where the cells elongate and rotate so that they are parallel to the lens surface.
[3] Lens fibers: The lens fibers are prismatic remnants of the subcapsular epithelium that have lost their nuclei and organelles. The lens fibers are filled with the cytoskeletal protein a, B, y-crystallin, which maintains the conformation and transparency of the lens. The newer lens fibers are located at the periphery of the lens, whereas the older lens fibers are displaced toward the center of the lens.
f. Retina: The innermost eye layer, the retina, is divided into two areas. The posterior two-thirds of the retina is a light-sensitive area called the pars optica. The anterior third is a light-insensitive area called the pars ciliaris and pars iridis. These two areas are separated by the ora serrata. The light-sensitive pars optica consists of the following 1 0 layers.
[1] Pigment epithelium: The pigment epithelium synthesizes and contains melanin, transports nutrients, phagocytizes shed tips of rod outer segments, converts 11-trans retinal to 11-cis retinal, and forms the blood-retinal barrier through zonula occludens (tight junctions).
[2] Photoreceptor layer: The photoreceptor layer consists of the outer segments, connecting cilium, and inner segments of rods and cones.
[3] Outer limiting membrane: The outer limiting membrane consists of zonula adherens between rods/cones and MOiier cells.
[4] Outer nuclear layer: The outer nuclear layer consists of nuclei of rods and cones.
[5] Outer plexiform layer: The outer plexiform layer consists of synapses between bipolar cells and horizontal cells with rods and cones.
[6] Inner nuclear layer: The inner nuclear layer consists of nuclei of horizontal cells, bipolar cells, amacrine cells, and Muller cells.
[7] Inner plexiform layer: The inner plexiform layer consists of synapses between bipolar cells and amacrine cells with ganglion cells.
[8] Ganglion cell layer: The ganglion cell layer consists of nuclei of ganglion cells.
[9] Optic nerve axon layer: The optic nerve axon layer consists of unmyelinated axons of ganglion cells.
[10] Inner limiting membrane: The inner limiting membrane consists of the termination of Muller cells and their basal lamina.
3. Musculature: The eye has both intrinsic and extrinsic muscles (Fig. 9). Intrinsic muscles include the pupillary sphincter and dilator as well as the ciliary muscle, which have been described previously. This section focuses on the attachments, functions, and innervations of the six extraocular muscles: medial rectus, lateral rectus, superior rectus, inferior rectus, superior oblique, and inferior oblique .
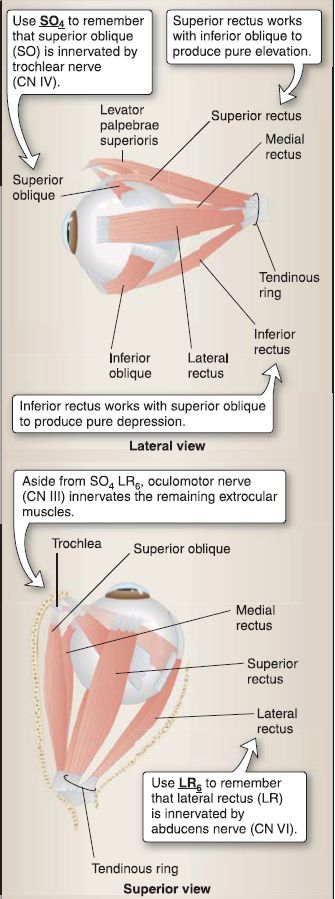
Figure 9: Extraocular muscles.
a. Movement: Unlike most of the pharyngeal-derived musculature of the head and neck, the six extraocular muscles arise embryologically from myotomes. They function, often in pairs, to allow for specific movements of the eye in various directions and planes. To understand their synchronous actions, it is important to understand that the eye moves around three axes (Fig. 10).

Figure 10: Eye movements.
[1] Anterior/posterior: Movement around this axis results in medial (intorsion) and lateral (extorsion) rotation.
[2] Horizontal: Movement around this axis results in elevation and depression.
[3] Vertical: Movement around this axis results in abduction and adduction.
b. Function: Due to the position of the eye in the orbit, only the medial and lateral rectus act to move the eye around one axis-the vertical-producing pure adduction and abduction, respectively. The other four muscles do not run in parallel with the eye and, therefore, produce movements around all three axes. These four muscles function in pairs to produce pure elevation and depression of the eye, where secondary and tertiary movements are cancelled out. The superior rectus and inferior oblique function
together to produce pure elevation, while the inferior rectus and superior oblique function together to produce pure depression.
[1] Superior rectus: This muscle elevates, abducts, and medially rotates the eye.
[2] Inferior rectus: This muscle depresses, adducts, and laterally rotates the eye.
[3] Superior oblique: This muscle depresses, abducts, and medially rotates the eye.
[4] Inferior oblique: This muscle elevates, adducts, and laterally rotates the eye.
4. Innervation: Five CNs (CNs II, 111, IV, V1, VI) enter the orbit to innervate structures associated with the eye (Fig. 11).
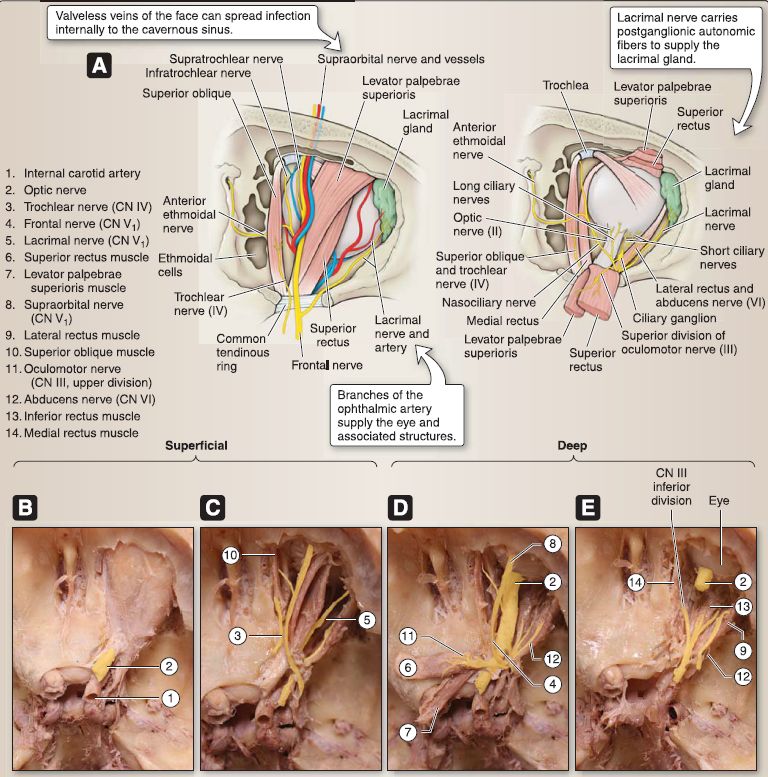
Figure 11: Superior view of orbit, superficial to deep. A, Schematics. B-E, Gross specimens.
a. Special senses (vision): The largest of these is the optic nerve (CN II), which traverses the optic canals as anterior extensions of the forebrain to mediate vision. The optic sheath, a covering made up of cranial dura and arachnoid mater layers, surrounds the nerve and is continuous with the fascia of the sclera.
b. Somatic motor and sensory: As shown in Figure 9, the medial rectus, superior rectus, inferior rectus, and inferior oblique muscles are innervated by the oculomotor nerve (CN Ill). The superior oblique and the lateral rectus are innervated by the trochlear nerve (CN IV) and abducens nerve (CN VI), respectively. The nasociliary nerve of V1 mediates somatic sensory to the eyeball.
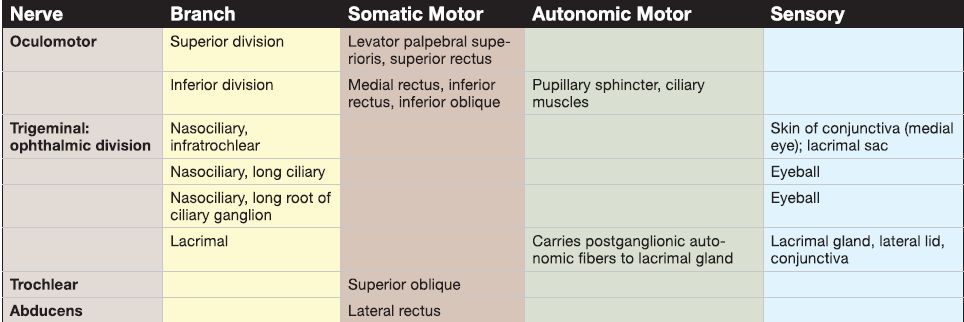
c. Autonomic motor: Postganglionic sympathetic fibers arise from the superior cervical ganglion and travel with the long ciliary nerve to provide autonomic motor innervation to the dilator pupillae and autonomic sensory to the iris and cornea. Postganglionic sympathetic fibers also travel with the lacrimal nerve to reach the lacrimal gland. Preganglionic parasympathetic fibers travel in CN Ill to the ciliary ganglion where they synapse on postganglionic parasympathetic neurons. Postganglionic parasympathetic fibers distribute to the ciliary muscles and sphincter pupillae muscles. Postganglionic parasympathetic fibers also arise from the pterygopalatine ganglion and travel from the zygomatic branch of V2 to the lacrimal nerve of V1 to reach the lacrimal gland. Innervation details are listed in Table 1.
Table 1: Nerves of the Eye
5. Arterial supply: Blood supply to the eye and structures housed in the orbit occurs primarily by way of the ophthalmic artery, a branch of the internal carotid artery. The ophthalmic artery travels with the optic nerve (CN II} through the optic canal to enter the orbit posteriorly. In the orbit, it gives off a series of branches including ethmoid air cell branches, supratrochlear, supraorbital, and retinal arteries.
6. Venous supply: Venous drainage occurs by way of the valveless superior and inferior ophthalmic veins, which communicate externally with the facial vein network and internally with the cavernous sinus and pterygoid venous plexus. Typically, the central retinal vein drains directly into the cavernous sinus.
 الاكثر قراءة في علم التشريح
الاكثر قراءة في علم التشريح
 اخر الاخبار
اخر الاخبار
اخبار العتبة العباسية المقدسة


