


 النبات
النبات
 الحيوان
الحيوان
 الأحياء المجهرية
الأحياء المجهرية
 علم الأمراض
علم الأمراض
 التقانة الإحيائية
التقانة الإحيائية
 التقنية الحيوية المكروبية
التقنية الحيوية المكروبية
 التقنية الحياتية النانوية
التقنية الحياتية النانوية
 علم الأجنة
علم الأجنة
 الأحياء الجزيئي
الأحياء الجزيئي
 علم وظائف الأعضاء
علم وظائف الأعضاء
 الغدد
الغدد
 المضادات الحيوية
المضادات الحيوية|
Read More
Date: 18-7-2021
Date: 5-11-2015
Date: 21-7-2021
|
Reproductive system
The process of sexual reproduction is a wonderful act in nature. This process, apart from ensuring a healthy progeny provides an opportunity to produce enormous range of genetically varied offspring. Organisms have adopted several strategies for sexual reproductive processes. Such adaptations have resulted in suitable morphological, anatomical and behavioral modifications. Human reproductive organs as internal and external genitalia are highly sophisticated yet simple in their functioning. The functioning is in accordance with psychological and endocrinological thresholds. An academic approach towards an understanding of the human male and female reproductive organs and their functions will go a long way in avoidance of unethical, unhealthy and unhygienic practices encountered at specific periods in life.
Male reproductive organs
The male reproductive system consists of the testes (singular: testis), epididymides (sing: epididymis), ductus deferentia or vasa deferentia (sing: ductus deferens, vas deferens), urethra, seminal vesicles, prostate gland, bulbourethral glands, scrotum and penis.
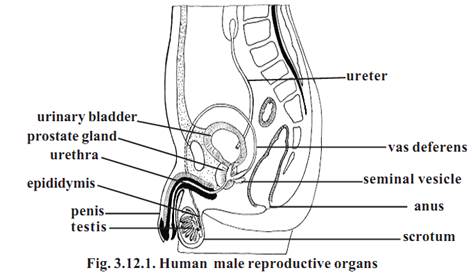
Testes : The testes are the primary reproductive organs or gonads in the male. These are suspended in the scrotum by scrotal tissues.
The sperm cells are temperature sensitive. They do not develop normally at usual body temperatures. Hence the testes and epididymides in which the sperm cells develop are located outside body cavity in the scrotum, where the temperature is low.
The left testis usually is 1 cm lower than the right. An average testis is 4-5 cm in length, 2-5cm in breadth. Its weight varies from 10.5-14g.
The outer part of each testis is a thick, white capsule called tunica albuginea. Internally the testis contains several incomplete septa. The septa divide each testis into about 300-400 cone shaped lobules. The lobules contain seminiferous tubules and interstitial cells or Leydig cells. Sperm cells develop within the seminiferous tubules.
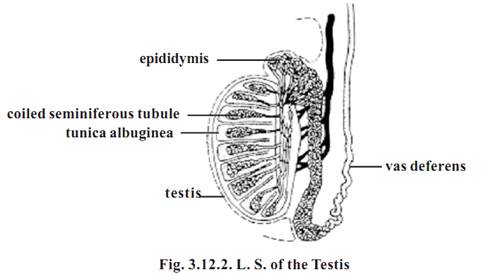
The seminiferous tubules are extensive. The combined length of the tubules in both testes is nearly 800 meters. These tubules through a set of short, straight tubules open into tubular network called the rete testis. The rete testis in turn open into efferent ductules. Internally the tubules and ductules are lined by ciliated columnar epithelium. These cells help to move the sperm cells out of the testis.
Epididymis: It is formed of extremely convoluted ductules coming out of the testis. It occurs on the posterior side of the testis. The maturation of sperm cells occurs within the ductules of the epididymis.
Vas deferens or ductus deferens: It emerges from the tail end of the
epididymis and ascends along the posterior side of the testis. It becomes associated with the blood vessels and nerves that supply the testis. Collectively these structures constitute the spermatic cord. Thus the spermatic cord consists of (1) Vas deferens (2) testicular artery and venus plexus (3) lymph vessels (4) nerves (5) fibrous processes and muscles. This cord enters into the pelvic region. The end of the vas deferns enlarges to form the ampulla. At this region the vas deferens is surrounded by smooth muscles capable of peristaltic contraction. They help to propel the sperm cells through the ductus deferens.
Ejaculatory duct: Nearer to the ampulla of each vas deferens there is a sac like seminal vesicle. It joins the ductus deferens to form the ejaculatory duct. These ducts are about 2.5 cm long. They project into the prostate gland and end by opening into the urethra.
Urethra: The male urethra extends from the urinary bladder to the distal end of the penis. It is about 20 cm long. It is a passageway for both urine and reproductive fluids. The urethra is divided into three parts. They are
1-The prostatic Urethra - It is closest to the bladder and passes through the prostate gland.
2-The membranous urethra - It is the shortest part of the urethra and it extends from the prostatic urethra.
3-The spongy urethra or penile urethra - It is the longest part of the urethra. It extends from the membranous urethra, through the length of the penis. There is several minute mucus secreting urethral glands opening into the urethral passage.
Penis - It is the male copulatory organ. It consists of two parts namely the radix or root and the corpus or body. The radix attaches the penis to the lower abdomen. The corpus is normally pendulous. It is covered by a loose skin.
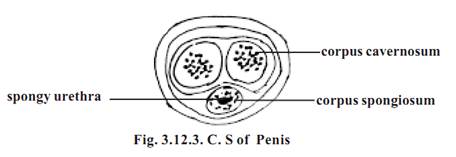
The corpus of the penis consists of three masses of erectile tissue. Flooding these tissues with blood causes the penis to enlarge and become firm. These tissues are the right and left corpora cavernosa and the median corpus spongiosum penis. Most of the corpus is formed of the corpora cavernoas. The corpus spongiosum penis surrounds the urethra and near the end of the penis it expands into a conical, glans penis. Its swollen base is the corona glandis.
The skin over the penis is thin. It is loosely connected to the tunica albuginea. At the tip of the penis it is folded to form the prepuce or the foreskin. It overlaps the glans penis. The corona glandis and penile neck have numerous preputial glands.
Seminal vesicles - These are two sac-like structures located between the bladder and rectum. Each vesicle is about 5 cm long. Their secretions contribute about 70% of the seminal fluid.
Prostate - It is a firm structure. It is partly glandular and partly fibromuscular. It is found around the beginning of the male urethra. It is about 3 cm in diameter. It weighs about 8g.
The muscular part of the prostate may help in dilating the urethra to hold the seminal fluid (3-5ml) during the period of sexual excitement prior to ejaculation.
After the middle age the prostate often enlarges. It may project into the bladder and interrupt urination.
Bulbourethral gland - These are two glands. They are small round masses about 1 cm in diameter. They lie lateral to the membranous urethra. Its secretion may control genitourinary diseases.
Scrotum - It is a fibromuscular sac. It contains the testes and their associated ducts. It is divided into right and left by cutaneous raphe. Its left side is usually lower. The external appearance varies according to age and body temperature. The scrotal skin is thin and pigmented. It has numerous sweat glands and nerve endings.
Female reproductive organs
In human female the internal reproductive organs are the ovaries, uterus, uterine tubes and vagina. Externally the organs are the mons pubis, labia major and labia minora, clitoris and vestibular glands.
Ovaries - These are paired structures. The two ovaries are placed on each side of the uterus in the pelvic region. They are greyish pink in colour. Each ovary is almond shaped. They are about 3cm long,1.5cm wide and 1cm thick.
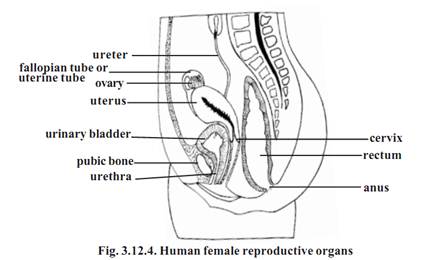
The ovary is attached to the posterior surface of the inner body wall by a membranous fold called the mesovarium. The ovary is further supported by suspensory and ovarian ligaments.
Ovarian structure - In young female the surface of the ovary is covered by a layer of ovarian surface epithelium. It consists of a single layer of cuboidal cells. Beneath the epithelium the ovary is surrounded by a tough coat named tunica albuginea. It is made of collagenous tissue.
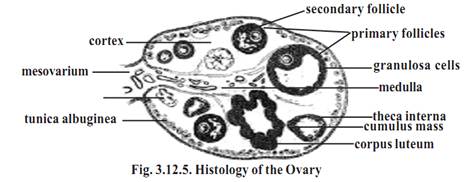
The ovary proper is divisible into two regions, namely the cortex and the medulla. The cortex region contains the ovarian follicles. The medulla is interior. It receives blood vessels and nerves at the hilum.
After puberty the cortex forms the major part of the ovary. It contains ovarian follicles and corpora lutea of various sizes. Their size depends on the stage of menstrual cycle or age. The cortex is filled with stroma composed of collagen. The follicles are embedded in the stroma.
Ovarian follicles
The formation of the female gamete has many different phases and it is complex. At birth, the primordial follicles are found in the superficial zone of the cortex. They contain primary oocytes (about 25mm in diameter). Each one of them is surrounded by a single layer of flat follicular cells. The follicles undergo changes as the female attains puberty. The various follicular stages are:
1-Primary follicle - The follicle cells are converted from squamous to cuboidal cells. The follicular membrane or membrana granulosa becomes multilayered. The oocyte increases in size. It has an outer thick layer called the zona pellucida. The follicular cells divide and form granulosa cells
2-Secondary follicle - It is about 20µm thick. The granulosa cells surround the oocyte and form a mound of cells called the cumulus ovaricus. The inner and outer theca become prominent. The theca interna is well established
3-Tertiary follicle - Only one follicle reaches the tertiary stage. It increases in size (2mm diameter). Now it is called the graffian follicle. The oocyte and ring of cells surrounding the oocyte (corona radiata) break away and float freely in the follicular fluid. Finally the wall of the follicle ruptures and the contents are released into the peritoneum.
The ovary of the foetus at 5 months gestation has 7 million oocytes. At birth the ovary of the child contains about 1 million oocytes. Due to further degeneration at the time of puberty only about 40,000 oocytes remain. Of the 40,000 oocytes only about 400 undergo ovulation during the reproductive years.
Corpus luteum - It is formed after ovulation. The walls of the empty follicle collapses and fold extensively. The granulosa cells of the theca externa get enlarged.
They are now termed as luteal cells. They secrete hormones. In pregnancy the corpus luteum persists. Otherwise, it degenerates after 10-12 days. The connective tissue cells get enlarged. It becomes white in colour and is now called as the corpus albicans. In course of time it shrinks and disappears.
Uterine tubes (Fallopian tubes) - There are two uterine tubes or oviducts, one on each side of the uterus. Each one is associated with a ovary. Each tube is about 10 cm length. The terminal part of the tube is enlarged to form the infundibulum. It opens into the peritoneal cavity. The opening is called the ostium. The uterine tube consists of three parts. The part nearer to the infundibulum is called the ampulla. It is the longest part. That part of the tube nearer to the uterus is called the isthmus. It is narrow. The tubular part entering into the uterus is called the uterine or intramural part.
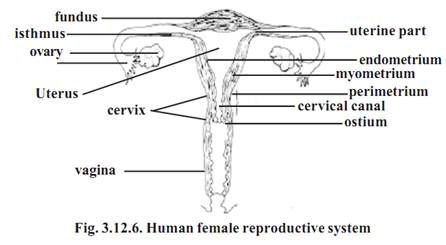
Uterus
It is a hollow thick walled muscular organ. It is pear shaped. It is about 7.5 cm long and 5 cm wide. It weighs about 50g.
During pregnancy its weight may go up to 1kg. Its larger rounded part is called as the fundus. The narrower part is called as the cervix. The cervix is directed inferiorly. The middle part is the body. The uterus continues as the cervical canal and opens into the vagina through a opening called the ostium.
The wall of the uterus is three layered. The outermost layer is the perimetrium or serous layer. The major part of the wall is made up of the next layer called the myometrium or muscular coat. The innermost layer is the endometrium or mucous membrane. The endometrium is a functional layer. It undergoes menstrual changes and sloughing during female sex cycle.
Vagina - It is the female copulatory organ. It is a fibromuscular tube. It is about 10 cm long. It extends from the uterus to the outside. The vaginal passage is used during intercourse and it allows menstrual flow and child birth.
External Genitalia
Vestibule - The external female genitalia is known as the vulva or pudendum. It consists of the vestibule and its surrounding structures. The vestibular region remains in between the two labia major. It contains the vaginal opening and the urethral opening. The vestibular region is surrounded by the mons pubis anteriorly and labia major and labia minora on the lateral sides.
Mons pubis - It is a rounded eminence situated anteriorly. It is made up of subcutaneous adipose connective tissue. It is covered by coarse hair at the time of puberty. It corresponds to similar structure in the male.
Labia majora - These are two longitudinal folds of skin. They form the outer boundary for the vestibule.
Labia minora - These two small skinfolds lie between the labia majora. They remain nearer to the vaginal opening.
Clitoris - It is homologues with male penis. It is an erectile structure. It is found in the anterior margin of the vestibule. It is a sensitive region having sensory receptors.
Hymen vaginae - It is a thin mucous membrane. It is found within the vaginal orifice or opening. If the membrane completely closes the vaginal opening, it should be removed to allow menstrual flow. In young women the hymen may normally get torn during physical exercise. In some women it may be absent. It has no established function.
External urethral opening - This opening is about 2.5 cm below the clitoris. It is anterior to the vaginal opening. It remains as a small cleft.
References
T. Sargunam Stephen, Biology (Zoology). First Edition – 2005, Government of Tamilnadu.



|
|
|
|
دراسة: عدم ترتيب الغرفة قد يدل على مشاكل نفسية
|
|
|
|
|
|
|
علماء: تغير المناخ تسبب في ارتفاع الحرارة خلال موسم الحج
|
|
|
|
|
|
|
عمره عام واحد ويعاني من ورم خبيث بوزن (3) كغم وعلى نفقة العتبة الحسينية ... مستشفى خديجة الكبرى (ع) ينجح باستئصال ورم سرطان الكلى لطفل من محافظة الأنبار
|
|
|